User:Madhero88/Pathophysiology of hypertension
The pathophysiology of hypertension is an area of active research, attempting to explain causes of hypertension, which is usually a chronic disease characterized by elevation of blood pressure to various degrees. Hypertension can be classified as either essential or secondary. Essential hypertension indicates that no specific medical cause can be found to explain a patient's condition. About 90-95% of hypertension is essential hypertension.[1][2][3][4] While secondary hypertension indicates that the high blood pressure is a result of another underlying condition, such as kidney disease or tumours (adrenal adenoma or pheochromocytoma). Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure and arterial aneurysm, and is a leading cause of chronic renal failure.[5]
Most mechanisms leading to secondary hypertension are well understood, while pathophysiology of essential hypertension remains an area of active research, with many theories and different links to many risk factors.
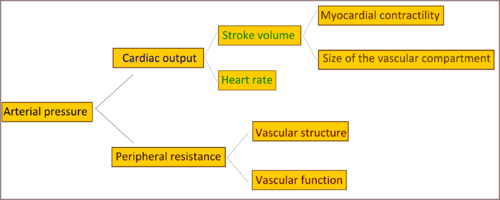
Cardiac output and peripheral resistance are the two determinants of arterial pressure. and so blood pressure is normally dependent on the balance between cardiac output and peripheral resistance.[6] Cardiac output is determined by stroke volume and heart rate; stroke volume is related to myocardial contractility and to the size of the vascular compartment. Peripheral resistance is determined by functional and anatomic changes in small arteries (lumen diameter 100–400 m) and arterioles.
Genetics[edit]
Evidence for genetic influence on blood pressure comes from various sources.[7] Its proved that there is greater similarity in blood pressure within families than between families, which indicates a form of inheritance.[8] And it was proved that wasnt due to shared environmental factors.[9] Single gene mutations is proved to cause Mendelian forms of high and low blood pressure.[10] almost 10 genes have been identified to cause this forms of hypertension.[10][11]These mutations affect blood pressure by altering renal salt handling.[12] Recently and with the aid of newly developed genetic analysis techniques researchers found statistically significant linkage of blood pressure to several chromosomal regions, including regions linked to familial combined hyperlipidemia.[13][14][15][16][17] These findings suggest that there are many genetic loci, each with small effects on blood pressure in the general population. Overall, however, identifiable single-gene causes of hypertension are uncommon, consistent with a multifactorial cause of essential hypertension.[2][7][18][19]
The best studied monogenic cause of hypertension is the Liddle syndrome, a rare but clinically important disorder in which constitutive activation of the epithelial sodium channel predisposes to severe, treatment-resistant hypertension.[20] Epithelial sodium channel activation resulting in inappropriate sodium retention at the renal collecting duct level. Patients with the Liddle syndrome typically present with volume-dependent, low renin, and low aldosterone, and hypertension. Screenings of general hypertensive populations indicate that the Liddle syndrome is rare and does not contribute substantially to the development of hypertension in the general population.[21]
Vascular volume[edit]
Vascular volume is a primary determinant of arterial pressure over the long term. Although the extracellular fluid space is composed of vascular and interstitial spaces, in general, alterations in total extracellular fluid volume are associated with proportional changes of blood volume. Sodium is predominantly an extracellular ion and is a primary determinant of the extracellular fluid volume. When NaCl intake exceeds the capacity of the kidney to excrete sodium, vascular volume initially expands and cardiac output increases. so the initial elevation of blood pressure in response to vascular volume expansion is related to an increase of cardiac output; however, over time, peripheral resistance increases and cardiac output reverts toward normal. As arterial pressure increases in response to a high NaCl intake, urinary sodium excretion increases and sodium balance is maintained at the expense of an increase in arterial pressure. The is due to a phenomenon called pressure-natriuresis(pressure induced diuresis), which may involve a subtle increase of glomerular filtration rate, decreased absorbing capacity of the renal tubules, and possibly hormonal factors such as atrial natriuretic factor. and as expected individuals with an impaired capacity to excrete sodium, require greater increases of arterial pressure to achieve natriuresis and sodium balance. So this can explain why patients with decreased capacity of the kidney to excrete sodium, due to either intrinsic renal disease or to increased production of a salt-retaining hormone (mineralocorticoid ie. aldosterone) resulting in increased renal tubular reabsorption of sodium will end up with NaCl(salt)-dependent hypertension.
Renin-angiotensin-aldosterone system[edit]
Another system maintaining the extracellular fluid volume, peripheral resistance and that if disturbed may lead to hypertension, is the renin-angiotensin-aldosterone system. Renin is a circulating enzyme that participates in maintaining extracellular volume, and arterial vasoconstriction, Thus it contributing to regulation of the blood pressure, it performs this function through breaking down (hydrolyzes) angiotensinogen secreted from the liver into the peptide angiotensin I, Angiotensin I is further cleaved by an enzyme that is located primarily but not exclusively in the pulmonary circulation bound to endothelium, that enzyme is angiotensin converting enzyme (ACE) producing angiotensin II, the most vasoactive peptide.[22][23]Angiotensin II is a potent constrictor of all blood vessels. It acts on the musculature of arteries and thereby raises the peripheral resistance, and so elevates blood pressure. Angiotensin II also acts on the adrenal glands too and releases Aldosterone, which stimulates the epithelial cells of the kidneys to increase re-absorption of salt and water leading to raised blood volume and raised blood pressure. So elevation of renin level in the blood, which is normally in adult human is 1.98-24.6 ng/L in the upright position.[24] will lead to hypertension.
Autonomic nervous system[edit]
Also the autonomic nervous system, plays a central role in maintaining the cardiovascular homeostasis via pressure, volume, and chemoreceptor signals. Done by altering peripheral vasculature, and kidneys, causing increased cardiac output, increased vascular resistance, and fluid retention. Disorder of the system, as in case of sympathetic nervous system overactivity, increases blood pressure and contributes to the development and maintenance of hypertension.[25][26] In addition, autonomic imbalance (ie. increased sympathetic tone accompanied by reduced parasympathetic tone) has been associated with many metabolic and hemodynamic abnormalities that result in increased cardiovascular morbidity and mortality.[27][25]
The mechanisms of increased sympathetic nervous system activity in hypertension are complex and involve alterations in baroreflex and chemoreflex pathways at both peripheral and central levels. Arterial baroreceptors are reset to a higher pressure in hypertensive patients, and this peripheral resetting reverts to normal when arterial pressure is normalized.[8][28][29] Furthermore, there is central resetting of the aortic baroreflex in hypertensive patients, resulting in suppression of sympathetic inhibition after activation of aortic baroreceptor nerves. This baroreflex resetting seems to be mediated, at least partly, by a central action of angiotensin II.[30][31] Additional small-molecule mediators that suppress baroreceptor activity and contribute to exaggerated sympathetic drive in hypertension include reactive oxygen species and endothelin.[32][33] Some studies shown that hypertensive patients manifest greater vasoconstrictor responses to infused norepinephrine than normotensive controls.[34] And that hypertensive patients doesn't show the normal response to increased circulating norepinephrine levels which generally induces downregulation of noradrenergic receptor, and its believed that this abnormal response is genetically inherited.[35]
Exposure to stress increases sympathetic outflow, and repeated stress-induced vasoconstriction may result in vascular hypertrophy, leading to progressive increases in peripheral resistance and blood pressure.[2] This could partly explain the greater incidence of hypertension in lower socioeconomic groups, since they must endure greater levels of stress associated with daily living. Persons with a family history of hypertension manifest augmented vasoconstrictor and sympathetic responses to laboratory stressors, such as cold pressor testing and mental stress, that may predispose them to hypertension. This is particularly true of young African Americans. Exaggerated stress responses may contribute to the increased incidence of hypertension in this group.[36]
Endothelial dysfunction[edit]
The endothelium of blood vessels produces an extensive range of substances that influence blood flow and, in turn, is affected by changes in the blood and the pressure of blood flow. For example, local nitric oxide and endothelin, which are secreted by the endothelium, are the major regulators of vascular tone and blood pressure. In patients with essential hypertension, the balance between the vasodilators and the vasoconstrictors is upset, which leads to changes in the endothelium and sets up a “vicious cycle” that contributes to the maintenance of high blood pressure. In patients with hypertension, endothelial activation and damage also lead to changes in vascular tone, vascular reactivity, and coagulation and fibrinolytic pathways. Alterations in endothelial function are a reliable indicator of target organ damage and atherosclerotic disease, as well as prognosis.[37]
References[edit]
- ^ Carretero OA, Oparil S (January 2000). "Essential hypertension. Part I: definition and etiology". Circulation. 101 (3): 329–35. doi:10.1161/01.cir.101.3.329. PMID 10645931. Retrieved 2009-06-05.
{{cite journal}}: CS1 maint: date and year (link) - ^ a b c Oparil S, Zaman MA, Calhoun DA (November 2003). "Pathogenesis of hypertension". Ann. Intern. Med. 139 (9): 761–76. doi:10.7326/0003-4819-139-9-200311040-00011. PMID 14597461.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) Cite error: The named reference "pmid14597461" was defined multiple times with different content (see the help page). - ^ Hall, John E.; Guyton, Arthur C. (2006). Textbook of medical physiology. St. Louis, Mo: Elsevier Saunders. p. 228. ISBN 0-7216-0240-1.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ "Hypertension: eMedicine Nephrology". Retrieved 2009-06-05.
- ^ Pierdomenico SD, Di Nicola M, Esposito AL; et al. (June 2009). "Prognostic Value of Different Indices of Blood Pressure Variability in Hypertensive Patients". American Journal of Hypertension. 22 (8): 842–847. doi:10.1038/ajh.2009.103. PMID 19498342. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Klabunde, Richard E. (2007). "Cardiovascular Physiology Concepts - Mean Arterial Pressure". Retrieved 2008-09-29.
- ^ a b Corvol P, Persu A, Gimenez-Roqueplo AP, Jeunemaitre X (June 1999). "Seven lessons from two candidate genes in human essential hypertension: angiotensinogen and epithelial sodium channel". Hypertension. 33 (6): 1324–31. doi:10.1161/01.hyp.33.6.1324. PMID 10373210. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b Feinleib M, Garrison RJ, Fabsitz R; et al. (October 1977). "The NHLBI twin study of cardiovascular disease risk factors: methodology and summary of results". American Journal of Epidemiology. 106 (4): 284–5. doi:10.1093/oxfordjournals.aje.a112464. PMID 562066. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) Cite error: The named reference "pmid" was defined multiple times with different content (see the help page). - ^ Biron P, Mongeau JG, Bertrand D (October 1976). "Familial aggregation of blood pressure in 558 adopted children". Canadian Medical Association Journal. 115 (8): 773–4. PMC 1878814. PMID 974967.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ a b Lifton RP, Gharavi AG, Geller DS (February 2001). "Molecular mechanisms of human hypertension". Cell. 104 (4): 545–56. doi:10.1016/s0092-8674(01)00241-0. PMID 11239411. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Wilson FH, Disse-Nicodème S, Choate KA; et al. (August 2001). "Human hypertension caused by mutations in WNK kinases". Science (New York, N.Y.). 293 (5532): 1107–12. doi:10.1126/science.1062844. PMID 11498583. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Guyton AC (June 1991). "Blood pressure control--special role of the kidneys and body fluids". Science (New York, N.Y.). 252 (5014): 1813–6. doi:10.1126/science.2063193. PMID 2063193. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) - ^ Hsueh WC, Mitchell BD, Schneider JL; et al. (June 2000). "QTL influencing blood pressure maps to the region of PPH1 on chromosome 2q31-34 in Old Order Amish". Circulation. 101 (24): 2810–6. doi:10.1161/01.cir.101.24.2810. PMID 10859286. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Levy D, DeStefano AL, Larson MG; et al. (October 2000). "Evidence for a gene influencing blood pressure on chromosome 17. Genome scan linkage results for longitudinal blood pressure phenotypes in subjects from the framingham heart study". Hypertension. 36 (4): 477–83. doi:10.1161/01.hyp.36.4.477. PMID 11040222. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Kristjansson K, Manolescu A, Kristinsson A; et al. (June 2002). "Linkage of essential hypertension to chromosome 18q". Hypertension. 39 (6): 1044–9. doi:10.1161/01.hyp.0000018580.24644.18. PMID 12052839. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Hunt SC, Ellison RC, Atwood LD, Pankow JS, Province MA, Leppert MF (July 2002). "Genome scans for blood pressure and hypertension: the National Heart, Lung, and Blood Institute Family Heart Study". Hypertension. 40 (1): 1–6. doi:10.1161/01.hyp.0000022660.28915.b1. PMID 12105129. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Selby JV, Newman B, Quiroga J, Christian JC, Austin MA, Fabsitz RR (April 1991). "Concordance for dyslipidemic hypertension in male twins". JAMA : the Journal of the American Medical Association. 265 (16): 2079–84. doi:10.1001/jama.1991.03460160057029. PMID 2013927.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Niu T, Yang J, Wang B; et al. (February 1999). "Angiotensinogen gene polymorphisms M235T/T174M: no excess transmission to hypertensive Chinese". Hypertension. 33 (2): 698–702. doi:10.1161/01.hyp.33.2.698. PMID 10024331. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Luft FC (May 2000). "Molecular genetics of human hypertension". Current Opinion in Nephrology and Hypertension. 9 (3): 259–66. doi:10.1097/00041552-200005000-00009. PMID 10847327. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) - ^ Shimkets RA, Warnock DG, Bositis CM; et al. (November 1994). "Liddle's syndrome: heritable human hypertension caused by mutations in the beta subunit of the epithelial sodium channel". Cell. 79 (3): 407–14. doi:10.1016/0092-8674(94)90250-x. PMID 7954808. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Melander O, Orho M, Fagerudd J; et al. (May 1998). "Mutations and variants of the epithelial sodium channel gene in Liddle's syndrome and primary hypertension". Hypertension. 31 (5): 1118–24. doi:10.1161/01.hyp.31.5.1118. PMID 9576123. Retrieved 2009-06-08.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Fujino T, Nakagawa N, Yuhki K; et al. (September 2004). "Decreased susceptibility to renovascular hypertension in mice lacking the prostaglandin I2 receptor IP". J. Clin. Invest. 114 (6): 805–12. doi:10.1172/JCI21382. PMC 516260. PMID 15372104.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Brenner & Rector's The Kidney, 7th ed., Saunders, 2004. pp.2118-2119.Full Text with MDConsult subscription
- ^ Hamilton Regional Laboratory Medicine Program - Laboratory Reference Centre Manual. Renin Direct
- ^ a b Esler M (June 2000). "The sympathetic system and hypertension". American Journal of Hypertension. 13 (6 Pt 2): 99S–105S. doi:10.1016/s0895-7061(00)00225-9. PMID 10921528.
{{cite journal}}: CS1 maint: date and year (link) - ^ Mark AL (December 1996). "The sympathetic nervous system in hypertension: a potential long-term regulator of arterial pressure". Journal of Hypertension. Supplement : Official Journal of the International Society of Hypertension. 14 (5): S159–65. PMID 9120673.
{{cite journal}}: CS1 maint: date and year (link) - ^ Brook RD, Julius S (June 2000). "Autonomic imbalance, hypertension, and cardiovascular risk". American Journal of Hypertension. 13 (6 Pt 2): 112S–122S. doi:10.1016/s0895-7061(00)00228-4. PMID 10921530.
{{cite journal}}: CS1 maint: date and year (link) - ^ Guo GB, Thames MD, Abboud FM (August 1983). "Arterial baroreflexes in renal hypertensive rabbits. Selectivity and redundancy of baroreceptor influence on heart rate, vascular resistance, and lumbar sympathetic nerve activity". Circulation Research. 53 (2): 223–34. doi:10.1161/01.res.53.2.223. PMID 6883646. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Xie PL, Chapleau MW, McDowell TS, Hajduczok G, Abboud FM (August 1990). "Mechanism of decreased baroreceptor activity in chronic hypertensive rabbits. Role of endogenous prostanoids". The Journal of Clinical Investigation. 86 (2): 625–30. doi:10.1172/JCI114754. PMC 296770. PMID 2117025. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Guo GB, Abboud FM (May 1984). "Impaired central mediation of the arterial baroreflex in chronic renal hypertension". The American Journal of Physiology. 246 (5 Pt 2): H720–7. doi:10.1152/ajpheart.1984.246.5.H720. PMID 6720985. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) - ^ Abboud FM (February 1974). "Effects of sodium, angiotensin, and steroids on vascular reactivity in man". Federation Proceedings. 33 (2): 143–9. PMID 4359754.
{{cite journal}}: CS1 maint: date and year (link) - ^ Li Z, Mao HZ, Abboud FM, Chapleau MW (October 1996). "Oxygen-derived free radicals contribute to baroreceptor dysfunction in atherosclerotic rabbits". Circulation Research. 79 (4): 802–11. doi:10.1161/01.res.79.4.802. PMID 8831504. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Chapleau MW, Hajduczok G, Abboud FM (July 1992). "Suppression of baroreceptor discharge by endothelin at high carotid sinus pressure". The American Journal of Physiology. 263 (1 Pt 2): R103–8. doi:10.1152/ajpregu.1992.263.1.R103. PMID 1636777. Retrieved 2009-06-08.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Ziegler MG, Mills P, Dimsdale JE (July 1991). "Hypertensives' pressor response to norepinephrine. Analysis by infusion rate and plasma levels". American Journal of Hypertension. 4 (7 Pt 1): 586–91. doi:10.1093/ajh/4.7.586. PMID 1873013.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Bianchetti MG, Beretta-Piccoli C, Weidmann P, Ferrier C (April 1986). "Blood pressure control in normotensive members of hypertensive families". Kidney International. 29 (4): 882–8. doi:10.1038/ki.1986.81. PMID 3520094.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Calhoun DA, Mutinga ML, Collins AS, Wyss JM, Oparil S (December 1993). "Normotensive blacks have heightened sympathetic response to cold pressor test". Hypertension. 22 (6): 801–5. doi:10.1161/01.hyp.22.6.801. PMID 8244512. Retrieved 2009-06-09.
{{cite journal}}: CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ O'Brien, Eoin; Beevers, D. G.; Lip, Gregory Y. H. (2007). ABC of hypertension. London: BMJ Books. ISBN 978-1-4051-3061-5.
{{cite book}}: CS1 maint: multiple names: authors list (link)
