Sexual addiction
This article may be too technical for most readers to understand. (May 2015) |
Sexual addiction, also known as sex addiction, is a state characterized by compulsive participation or engagement in sexual activity, particularly sexual intercourse, despite negative consequences.[1] Proponents of a diagnostic model for sexual addiction, as defined here, consider it to be one of several sex-related disorders within an umbrella concept known as hypersexual disorder.[2] In clinical diagnostics, the term sexual dependence may also refer to a conceptual model that is used to assess people who report being unable to control their sexual urges, behaviors, or thoughts. Related models of pathological sexual behavior include hypersexuality, erotomania, nymphomania, satyriasis, Don Juanism (or Don Juanitaism), and paraphilia-related disorders.[3][4][5]
Clinicians, such as psychiatrists, sociologists, sexologists, and other specialists, have differing opinions on the classification and clinical diagnosis of sexual addiction. As a result, "sexual addiction" does not exist as a clinical entity in either the DSM or ICD medical classifications of diseases and medical disorders.
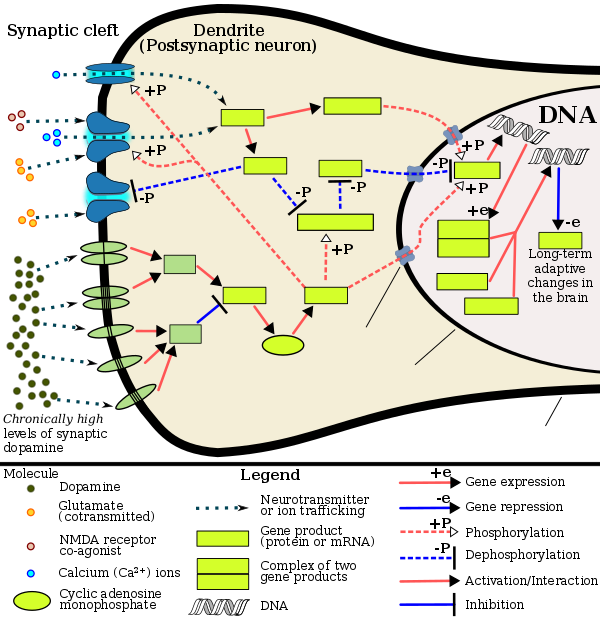
Neuroscientists, pharmacologists, molecular biologists, and other researchers in related fields have identified a transcriptional and epigenetic model of drug and behavioral (including sexual) addiction pathophysiology. Diagnostic models, which use the pharmacological model of addiction (this model associates addiction with drug-related concepts, particularly physical dependence, drug withdrawal, and drug tolerance[6]), do not currently include diagnostic criteria to identify sexual addictions in a clinical setting. In the alternative reward-reinforcement model of addiction, which uses neuropsychological concepts to characterize addictions, sexual addictions are identifiable and well-characterized.[7][8] In this model, addictive drugs are characterized as those which are both reinforcing and rewarding (i.e., activates neural pathways associated with reward perception).[6] Addictive behaviors (those which can induce a compulsive state) are similarly identified and characterized by their rewarding and reinforcing properties.
Mechanisms
Current research on sexual addiction within the context of the reward-reinforcement model indicates that it is well-characterized as an addiction (in this context, a compulsive behavior)[7][8] and that it develops through the same biomolecular mechanisms that induce drug addictions;[7][9] specifically, sexual activity has been shown to be highly rewarding[8][9] and naturally reinforcing.[8][9] Excessive activation of the associated reward-reinforcement mechanisms has been directly implicated in the development of compulsive (i.e., an addiction to) sexual behavior.[7][8]
In humans, a dopamine dysregulation syndrome, characterized by drug-induced compulsive engagement in sexual activity or gambling, has also been observed in some individuals taking dopaminergic medications.[7] Current experimental models of addiction to natural rewards and drug reward demonstrate common alterations in gene expression in the mesocorticolimbic projection.[7][10] ΔFosB is the most significant gene transcription factor involved in addiction, since its viral or genetic overexpression in the nucleus accumbens is necessary and sufficient for most of the neural adaptations and plasticity that occur;[10] it has been implicated in addictions to alcohol, cannabinoids, cocaine, nicotine, opioids, phenylcyclidine, and substituted amphetamines.[7][10][11] ΔJunD is the transcription factor which directly opposes ΔFosB.[10] Increases in nucleus accumbens ΔJunD expression can reduce or, with a large increase, even block most of the neural alterations seen in chronic drug abuse (i.e., the alterations mediated by ΔFosB).[10]
ΔFosB also plays an important role in regulating behavioral responses to natural rewards, such as palatable food, sex, and exercise.[8][10] Natural rewards, like drugs of abuse, induce ΔFosB in the nucleus accumbens, and chronic acquisition of these rewards can result in a similar pathological addictive state.[7][8] Thus, ΔFosB is also the key transcription factor involved in addictions to natural rewards as well,[7][9] and sex addictions in particular, since ΔFosB in the nucleus accumbens is critical for the reinforcing effects of sexual reward.[8] Research on the interaction between natural and drug rewards suggests that psychostimulants and sexual reward possess cross-sensitization effects and act on common biomolecular mechanisms of addiction-related neuroplasticity which are mediated through ΔFosB.[7][9]
ΔFosB inhibitors (drugs[which?] or treatments[which?] that oppose its action) may be an effective treatment for addiction and addictive disorders.[12]
| sexual addiction | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | sex addiction | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | GeneCards: [1]; OMA:- orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Protein fosB, also known as FosB and G0/G1 switch regulatory protein 3 (G0S3), is a protein that in humans is encoded by the FBJ murine osteosarcoma viral oncogene homolog B (FOSB) gene.[13][14][15]
The FOS gene family consists of four members: FOS, FOSB, FOSL1, and FOSL2. These genes encode leucine zipper proteins that can dimerize with proteins of the JUN family (e.g., c-Jun, JunD), thereby forming the transcription factor complex AP-1. As such, the FOS proteins have been implicated as regulators of cell proliferation, differentiation, and transformation.[13] FosB and its truncated splice variants, ΔFosB and further truncated Δ2ΔFosB, are all involved in osteosclerosis, although Δ2ΔFosB lacks a known transactivation domain, in turn preventing it from affecting transcription through the AP-1 complex.[16]
The ΔFosB splice variant has been identified as playing a central, crucial[17][10] role in the development and maintenance of addiction.[17][7][18] ΔFosB overexpression (i.e., an abnormally and excessively high level of ΔFosB expression which produces a pronounced gene-related phenotype) triggers the development of addiction-related neuroplasticity throughout the reward system and produces a behavioral phenotype that is characteristic of an addiction.[17][18][19] ΔFosB differs from the full length FosB and further truncated Δ2ΔFosB in its capacity to produce these effects, as only accumbal ΔFosB overexpression is associated with pathological responses to drugs.[20]
DeltaFosB
DeltaFosB – more commonly written as ΔFosB – is a truncated splice variant of the FOSB gene.[21] ΔFosB has been implicated as a critical factor in the development of virtually all forms of behavioral and drug addictions.[10][7][8] In the brain's reward system, it is linked to changes in a number of other gene products, such as CREB and sirtuins.[22][23][24] In the body, ΔFosB regulates the commitment of mesenchymal precursor cells to the adipocyte or osteoblast lineage.[25]
In the nucleus accumbens, ΔFosB functions as a "sustained molecular switch" and "master control protein" in the development of an addiction.[17][26][27] In other words, once "turned on" (sufficiently overexpressed) ΔFosB triggers a series of transcription events that ultimately produce an addictive state (i.e., compulsive reward-seeking involving a particular stimulus); this state is sustained for months after cessation of drug use due to the abnormal and exceptionally long half-life of ΔFosB isoforms.[17][26][27] ΔFosB expression in D1-type nucleus accumbens medium spiny neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement while decreasing sensitivity to aversion.[17][18] Based upon the accumulated evidence, a medical review from late 2014 argued that accumbal ΔFosB expression can be used as an addiction biomarker and that the degree of accumbal ΔFosB induction by a drug is a metric for how addictive it is relative to others.[17]
Chronic administration of anandamide, or N-arachidonylethanolamide (AEA), an endogenous cannabinoid, and additives such as sucralose, a noncaloric sweetener used in many food products of daily intake, are found to induce an overexpression of ΔFosB in the infralimbic cortex (Cx), nucleus accumbens (NAc) core, shell, and central nucleus of amygdala (Amy), that induce long-term changes in the reward system.[28]
Role in addiction
| Addiction and dependence glossary[18][29][30] | |
|---|---|
| |
Chronic addictive drug use causes alterations in gene expression in the mesocorticolimbic projection, which arise through transcriptional and epigenetic mechanisms.[10][37][38] The most important transcription factors that produce these alterations are ΔFosB, cyclic adenosine monophosphate (cAMP) response element binding protein (CREB), and nuclear factor kappa B (NF-κB).[10] ΔFosB is the most significant biomolecular mechanism in addiction because the overexpression of ΔFosB in the D1-type medium spiny neurons in the nucleus accumbens is necessary and sufficient for many of the neural adaptations and behavioral effects (e.g., expression-dependent increases in drug self-administration and reward sensitization) seen in drug addiction.[17][10][18] ΔFosB overexpression has been implicated in addictions to alcohol, cannabinoids, cocaine, methylphenidate, nicotine, opioids, phencyclidine, propofol, and substituted amphetamines, among others.[17][10][37][11][39] ΔJunD, a transcription factor, and G9a, a histone methyltransferase, both oppose the function of ΔFosB and inhibit increases in its expression.[10][18][40] Increases in nucleus accumbens ΔJunD expression (via viral vector-mediated gene transfer) or G9a expression (via pharmacological means) reduces, or with a large increase can even block, many of the neural and behavioral alterations seen in chronic drug abuse (i.e., the alterations mediated by ΔFosB).[19][10] Repression of c-Fos by ΔFosB, which consequently further induces expression of ΔFosB, forms a positive feedback loop that serves to indefinitely perpetuate the addictive state.
ΔFosB also plays an important role in regulating behavioral responses to natural rewards, such as palatable food, sex, and exercise.[10][8] Natural rewards, similar to drugs of abuse, induce gene expression of ΔFosB in the nucleus accumbens, and chronic acquisition of these rewards can result in a similar pathological addictive state through ΔFosB overexpression.[10][7][8] Consequently, ΔFosB is the key mechanism involved in addictions to natural rewards (i.e., behavioral addictions) as well;[10][7][8] in particular, ΔFosB in the nucleus accumbens is critical for the reinforcing effects of sexual reward.[8] Research on the interaction between natural and drug rewards suggests that dopaminergic psychostimulants (e.g., amphetamine) and sexual behavior act on similar biomolecular mechanisms to induce ΔFosB in the nucleus accumbens and possess bidirectional reward cross-sensitization effects[note 1] that are mediated through ΔFosB.[7][9] This phenomenon is notable since, in humans, a dopamine dysregulation syndrome, characterized by drug-induced compulsive engagement in natural rewards (specifically, sexual activity, shopping, and gambling), has also been observed in some individuals taking dopaminergic medications.[7]
ΔFosB inhibitors (drugs or treatments that oppose its action or reduce its expression) may be an effective treatment for addiction and addictive disorders.[12] Current medical reviews of research involving lab animals have identified a drug class – class I histone deacetylase inhibitors[note 2] – that indirectly inhibits the function and further increases in the expression of accumbal ΔFosB by inducing G9a expression in the nucleus accumbens after prolonged use.[19][40][41][42] These reviews and subsequent preliminary evidence which used oral administration or intraperitoneal administration of the sodium salt of butyric acid or other class I HDAC inhibitors for an extended period indicate that these drugs have efficacy in reducing addictive behavior in lab animals[note 3] that have developed addictions to ethanol, psychostimulants (i.e., amphetamine and cocaine), nicotine, and opiates;[40][42][43][44] however, as of August 2015[update], few clinical trials involving humans with addiction and any HDAC class I inhibitors have been conducted to test for treatment efficacy in humans or identify an optimal dosing regimen.[note 4]
Plasticity in cocaine addiction
ΔFosB accumulation from excessive drug use
Top: this depicts the initial effects of high dose exposure to an addictive drug on gene expression in the nucleus accumbens for various Fos family proteins (i.e., c-Fos, FosB, ΔFosB, Fra1, and Fra2).
Bottom: this illustrates the progressive increase in ΔFosB expression in the nucleus accumbens following repeated twice daily drug binges, where these phosphorylated (35–37 kilodalton) ΔFosB isoforms persist in the D1-type medium spiny neurons of the nucleus accumbens for up to 2 months.[27][35] |
ΔFosB levels have been found to increase upon the use of cocaine.[46] Each subsequent dose of cocaine continues to increase ΔFosB levels with no apparent ceiling of tolerance.[citation needed] Elevated levels of ΔFosB leads to increases in brain-derived neurotrophic factor (BDNF) levels, which in turn increases the number of dendritic branches and spines present on neurons involved with the nucleus accumbens and prefrontal cortex areas of the brain. This change can be identified rather quickly, and may be sustained weeks after the last dose of the drug.
Transgenic mice exhibiting inducible expression of ΔFosB primarily in the nucleus accumbens and dorsal striatum exhibit sensitized behavioural responses to cocaine.[47] They self-administer cocaine at lower doses than control,[48] but have a greater likelihood of relapse when the drug is withheld.[27][48] ΔFosB increases the expression of AMPA receptor subunit GluR2[47] and also decreases expression of dynorphin, thereby enhancing sensitivity to reward.[27]
| Target gene |
Target expression |
Neural effects | Behavioral effects |
|---|---|---|---|
| c-Fos | ↓ | Molecular switch enabling the chronic induction of ΔFosB[note 5] |
– |
| dynorphin | ↓ [note 6] |
• Downregulation of κ-opioid feedback loop | • Diminished self-extinguishing response to drug |
| NF-κB | ↑ | • Expansion of Nacc dendritic processes • NF-κB inflammatory response in the NAcc • NF-κB inflammatory response in the CP |
• Increased drug reward • Locomotor sensitization |
| GluR2 | ↑ | • Decreased sensitivity to glutamate | • Increased drug reward |
| Cdk5 | ↑ | • GluR1 synaptic protein phosphorylation • Expansion of NAcc dendritic processes |
• Decreased drug reward (net effect) |
| Form of neuroplasticity or behavioral plasticity |
Type of reinforcer | Sources | |||||
|---|---|---|---|---|---|---|---|
| Opiates | Psychostimulants | High fat or sugar food | Sexual intercourse | Physical exercise (aerobic) |
Environmental enrichment | ||
| ΔFosB expression in nucleus accumbens D1-type MSNs |
↑ | ↑ | ↑ | ↑ | ↑ | ↑ | [7] |
| Behavioral plasticity | |||||||
| Escalation of intake | Yes | Yes | Yes | [7] | |||
| Psychostimulant cross-sensitization |
Yes | Not applicable | Yes | Yes | Attenuated | Attenuated | [7] |
| Psychostimulant self-administration |
↑ | ↑ | ↓ | ↓ | ↓ | [7] | |
| Psychostimulant conditioned place preference |
↑ | ↑ | ↓ | ↑ | ↓ | ↑ | [7] |
| Reinstatement of drug-seeking behavior | ↑ | ↑ | ↓ | ↓ | [7] | ||
| Neurochemical plasticity | |||||||
| CREB phosphorylation in the nucleus accumbens |
↓ | ↓ | ↓ | ↓ | ↓ | [7] | |
| Sensitized dopamine response in the nucleus accumbens |
No | Yes | No | Yes | [7] | ||
| Altered striatal dopamine signaling | ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD2 | ↑DRD2 | [7] | |
| Altered striatal opioid signaling | No change or ↑μ-opioid receptors |
↑μ-opioid receptors ↑κ-opioid receptors |
↑μ-opioid receptors | ↑μ-opioid receptors | No change | No change | [7] |
| Changes in striatal opioid peptides | ↑dynorphin No change: enkephalin |
↑dynorphin | ↓enkephalin | ↑dynorphin | ↑dynorphin | [7] | |
| Mesocorticolimbic synaptic plasticity | |||||||
| Number of dendrites in the nucleus accumbens | ↓ | ↑ | ↑ | [7] | |||
| Dendritic spine density in the nucleus accumbens |
↓ | ↑ | ↑ | [7] | |||
Other functions in the brain
Viral overexpression of ΔFosB in the output neurons of the nigrostriatal dopamine pathway (i.e., the medium spiny neurons in the dorsal striatum) induces levodopa-induced dyskinesias in animal models of Parkinson's disease.[49][50] Dorsal striatal ΔFosB is overexpressed in rodents and primates with dyskinesias;[50] postmortem studies of individuals with Parkinson's disease that were treated with levodopa have also observed similar dorsal striatal ΔFosB overexpression.[50] Levetiracetam, an antiepileptic drug, has been shown to dose-dependently decrease the induction of dorsal striatal ΔFosB expression in rats when co-administered with levodopa;[50] the signal transduction involved in this effect is unknown.[50]
ΔFosB expression in the nucleus accumbens shell increases resilience to stress and is induced in this region by acute exposure to social defeat stress.[51][52][53]
Antipsychotic drugs have been shown to increase ΔFosB as well, more specifically in the prefrontal cortex. This increase has been found to be part of pathways for the negative side effects that such drugs produce.[54]
See also
Notes
- ^ In simplest terms, this means that when either amphetamine or sex is perceived as "more alluring or desirable" through reward sensitization, this effect occurs with the other as well.
- ^ Inhibitors of class I histone deacetylase (HDAC) enzymes are drugs that inhibit four specific histone-modifying enzymes: HDAC1, HDAC2, HDAC3, and HDAC8. Most of the animal research with HDAC inhibitors has been conducted with four drugs: butyrate salts (mainly sodium butyrate), trichostatin A, valproic acid, and SAHA;[41][42] butyric acid is a naturally occurring short-chain fatty acid in humans, while the latter two compounds are FDA-approved drugs with medical indications unrelated to addiction.
- ^ Specifically, prolonged administration of a class I HDAC inhibitor appears to reduce an animal's motivation to acquire and use an addictive drug without affecting an animals motivation to attain other rewards (i.e., it does not appear to cause motivational anhedonia) and reduce the amount of the drug that is self-administered when it is readily available.[40][42][43]
- ^ Among the few clinical trials that employed a class I HDAC inhibitor, one utilized valproate for methamphetamine addiction.[45]
- ^ In other words, c-Fos repression allows ΔFosB to accumulate within nucleus accumbens medium spiny neurons more rapidly because it is selectively induced in this state.[18]
- ^ ΔFosB has been implicated in causing both increases and decreases in dynorphin expression in different studies;[17][22] this table entry reflects only a decrease.
- Image legend
- ^ (Text color) Transcription factors
References
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 364–365, 375. ISBN 9780071481274.
The defining feature of addiction is compulsive, out-of-control drug use, despite negative consequences. ...
compulsive eating, shopping, gambling, and sex–so-called "natural addictions"– ... Indeed, addiction to both drugs and behavioral rewards may arise from similar dysregulation of the mesolimbic dopamine system. - ^ Karila L, Wéry A, Weinstein A, Cottencin O, Petit A, Reynaud M, Billieux J (2014). "Sexual addiction or hypersexual disorder: different terms for the same problem? A review of the literature". Curr. Pharm. Des. 20 (25): 4012–20. doi:10.2174/13816128113199990619. PMID 24001295.
Sexual addiction, which is also known as hypersexual disorder, has largely been ignored by psychiatrists, even though the condition causes serious psychosocial problems for many people. A lack of empirical evidence on sexual addiction is the result of the disease's complete absence from versions of the Diagnostic and Statistical Manual of Mental Disorders. ... Existing prevalence rates of sexual addiction-related disorders range from 3% to 6%. Sexual addiction/hypersexual disorder is used as an umbrella construct to encompass various types of problematic behaviors, including excessive masturbation, cybersex, pornography use, sexual behavior with consenting adults, telephone sex, strip club visitation, and other behaviors. The adverse consequences of sexual addiction are similar to the consequences of other addictive disorders. Addictive, somatic and psychiatric disorders coexist with sexual addiction. In recent years, research on sexual addiction has proliferated, and screening instruments have increasingly been developed to diagnose or quantify sexual addiction disorders. In our systematic review of the existing measures, 22 questionnaires were identified. As with other behavioral addictions, the appropriate treatment of sexual addiction should combine pharmacological and psychological approaches.
- ^ Coleman, Eli (June–July 2003). "Compulsive Sexual Behavior: What to Call It, How to Treat It?" (PDF). SIECUS Report. The Debate: Sexual Addiction and Compulsion. 31 (5). ProQuest Academic Research Library: 12–16. Retrieved 15 October 2012.
- ^ Coleman, E. (2011). "Chapter 28. Impulsive/compulsive sexual behavior: Assessment and treatment". In Grant, Jon E.; Potenza, Marc N. (eds.). The Oxford Handbook of Impulse Control Disorders. New York: Oxford University Press. p. 375. ISBN 9780195389715.
- ^ Carnes, Patrick (1994). Contrary to Love: Helping the Sexual Addict. Hazelden Publishing. p. 28. ISBN 1568380593.
- ^ a b Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 364–368. ISBN 9780071481274.
The defining feature of addiction is compulsive, out-of-control drug use, despite negative consequences. ...Addictive drugs are both rewarding and reinforcing. A reward is a stimulus that the brain interprets as intrinsically positive or as something to be approached. A reinforcing stimulus is one that increases the probability that behaviors paired with it will be repeated. Not all reinforcers are rewarding; for example, a negative or punishing stimulus might reinforce avoidance behaviors. ... Familiar pharmacologic terms such as tolerance, dependence, and sensitization are useful in describing some of the time-dependent processes that underlie addiction. ...
Dependence is defined as an adaptive state that develops in response to repeated drug administration, and is unmasked during withdrawal, which occurs when drug taking stops. Dependence from long-term drug use may have both a somatic component, manifested by physical symptoms, and an emotional–motivation component, manifested by dysphoria. While physical dependence and withdrawal occur with some drugs of abuse (opiates, ethanol), these phenomena are not useful in the diagnosis of addiction because they do not occur with other drugs of abuse (cocaine, amphetamine) and can occur with many drugs that are not abused (propranolol, clonidine). The official diagnosis of drug addiction by the Diagnostic and Statistic Manual of Mental Disorders (2000), which makes distinctions between drug use, abuse, and substance dependence, is flawed. First, diagnosis of drug use versus abuse can be arbitrary and reflect cultural norms, not medical phenomena. Second, the term substance dependence implies that dependence is the primary pharmacologic phenomenon underlying addiction, which is likely not true, as tolerance, sensitization, and learning and memory also play central roles. It is ironic and unfornate that the Manual avoids use of the term addiction, which provides the best description of the clinical syndrome. - ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac Olsen CM (December 2011). "Natural rewards, neuroplasticity, and non-drug addictions". Neuropharmacology. 61 (7): 1109–1122. doi:10.1016/j.neuropharm.2011.03.010. PMC 3139704. PMID 21459101.
Cross-sensitization is also bidirectional, as a history of amphetamine administration facilitates sexual behavior and enhances the associated increase in NAc DA ... As described for food reward, sexual experience can also lead to activation of plasticity-related signaling cascades. The transcription factor delta FosB is increased in the NAc, PFC, dorsal striatum, and VTA following repeated sexual behavior (Wallace et al., 2008; Pitchers et al., 2010b). This natural increase in delta FosB or viral overexpression of delta FosB within the NAc modulates sexual performance, and NAc blockade of delta FosB attenuates this behavior (Hedges et al, 2009; Pitchers et al., 2010b). Further, viral overexpression of delta FosB enhances the conditioned place preference for an environment paired with sexual experience (Hedges et al., 2009). ... In some people, there is a transition from "normal" to compulsive engagement in natural rewards (such as food or sex), a condition that some have termed behavioral or non-drug addictions (Holden, 2001; Grant et al., 2006a). ... In humans, the role of dopamine signaling in incentive-sensitization processes has recently been highlighted by the observation of a dopamine dysregulation syndrome in some patients taking dopaminergic drugs. This syndrome is characterized by a medication-induced increase in (or compulsive) engagement in non-drug rewards such as gambling, shopping, or sex (Evans et al, 2006; Aiken, 2007; Lader, 2008)."
Table 1" Cite error: The named reference "Natural and drug addictions" was defined multiple times with different content (see the help page). - ^ a b c d e f g h i j k l m Blum K, Werner T, Carnes S, Carnes P, Bowirrat A, Giordano J, Oscar-Berman M, Gold M (2012). "Sex, drugs, and rock 'n' roll: hypothesizing common mesolimbic activation as a function of reward gene polymorphisms". J. Psychoactive Drugs. 44 (1): 38–55. doi:10.1080/02791072.2012.662112. PMC 4040958. PMID 22641964.
It has been found that deltaFosB gene in the NAc is critical for reinforcing effects of sexual reward. Pitchers and colleagues (2010) reported that sexual experience was shown to cause DeltaFosB accumulation in several limbic brain regions including the NAc, medial pre-frontal cortex, VTA, caudate, and putamen, but not the medial preoptic nucleus. Next, the induction of c-Fos, a downstream (repressed) target of DeltaFosB, was measured in sexually experienced and naive animals. The number of mating-induced c-Fos-IR cells was significantly decreased in sexually experienced animals compared to sexually naive controls. Finally, DeltaFosB levels and its activity in the NAc were manipulated using viral-mediated gene transfer to study its potential role in mediating sexual experience and experience-induced facilitation of sexual performance. Animals with DeltaFosB overexpression displayed enhanced facilitation of sexual performance with sexual experience relative to controls. In contrast, the expression of DeltaJunD, a dominant-negative binding partner of DeltaFosB, attenuated sexual experience-induced facilitation of sexual performance, and stunted long-term maintenance of facilitation compared to DeltaFosB overexpressing group. Together, these findings support a critical role for DeltaFosB expression in the NAc in the reinforcing effects of sexual behavior and sexual experience-induced facilitation of sexual performance. ... both drug addiction and sexual addiction represent pathological forms of neuroplasticity along with the emergence of aberrant behaviors involving a cascade of neurochemical changes mainly in the brain's rewarding circuitry.
Cite error: The named reference "ΔFosB reward" was defined multiple times with different content (see the help page). - ^ a b c d e f Pitchers KK, Vialou V, Nestler EJ, Laviolette SR, Lehman MN, Coolen LM (February 2013). "Natural and drug rewards act on common neural plasticity mechanisms with ΔFosB as a key mediator". J. Neurosci. 33 (8): 3434–3442. doi:10.1523/JNEUROSCI.4881-12.2013. PMC 3865508. PMID 23426671.
Drugs of abuse induce neuroplasticity in the natural reward pathway, specifically the nucleus accumbens (NAc), thereby causing development and expression of addictive behavior. ... Together, these findings demonstrate that drugs of abuse and natural reward behaviors act on common molecular and cellular mechanisms of plasticity that control vulnerability to drug addiction, and that this increased vulnerability is mediated by ΔFosB and its downstream transcriptional targets. ... Sexual behavior is highly rewarding (Tenk et al., 2009), and sexual experience causes sensitized drug-related behaviors, including cross-sensitization to amphetamine (Amph)-induced locomotor activity (Bradley and Meisel, 2001; Pitchers et al., 2010a) and enhanced Amph reward (Pitchers et al., 2010a). Moreover, sexual experience induces neural plasticity in the NAc similar to that induced by psychostimulant exposure, including increased dendritic spine density (Meisel and Mullins, 2006; Pitchers et al., 2010a), altered glutamate receptor trafficking, and decreased synaptic strength in prefrontal cortex-responding NAc shell neurons (Pitchers et al., 2012). Finally, periods of abstinence from sexual experience were found to be critical for enhanced Amph reward, NAc spinogenesis (Pitchers et al., 2010a), and glutamate receptor trafficking (Pitchers et al., 2012). These findings suggest that natural and drug reward experiences share common mechanisms of neural plasticity
Cite error: The named reference "Amph and sex addiction" was defined multiple times with different content (see the help page). - ^ a b c d e f g h i j k l m n o p q Nestler EJ (December 2012). "Transcriptional mechanisms of drug addiction". Clin. Psychopharmacol. Neurosci. 10 (3): 136–143. doi:10.9758/cpn.2012.10.3.136. PMC 3569166. PMID 23430970.
ΔFosB has been linked directly to several addiction-related behaviors ... Importantly, genetic or viral overexpression of ΔJunD, a dominant negative mutant of JunD which antagonizes ΔFosB- and other AP-1-mediated transcriptional activity, in the NAc or OFC blocks these key effects of drug exposure14,22–24. This indicates that ΔFosB is both necessary and sufficient for many of the changes wrought in the brain by chronic drug exposure. ΔFosB is also induced in D1-type NAc MSNs by chronic consumption of several natural rewards, including sucrose, high fat food, sex, wheel running, where it promotes that consumption14,26–30. This implicates ΔFosB in the regulation of natural rewards under normal conditions and perhaps during pathological addictive-like states.
Cite error: The named reference "Nestler" was defined multiple times with different content (see the help page). - ^ a b Kanehisa Laboratories (2 August 2013). "Alcoholism – Homo sapiens (human)". KEGG Pathway. Retrieved 10 April 2014. Cite error: The named reference "Alcoholism ΔFosB" was defined multiple times with different content (see the help page).
- ^ a b Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and addictive disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 384–385. ISBN 9780071481274. Cite error: The named reference "Malenka_2009_04" was defined multiple times with different content (see the help page).
- ^ a b "Entrez Gene: FOSB FBJ murine osteosarcoma viral oncogene homolog B".
- ^ Siderovski DP, Blum S, Forsdyke RE, Forsdyke DR (October 1990). "A set of human putative lymphocyte G0/G1 switch genes includes genes homologous to rodent cytokine and zinc finger protein-encoding genes". DNA and Cell Biology. 9 (8): 579–87. doi:10.1089/dna.1990.9.579. PMID 1702972.
- ^ Martin-Gallardo A, McCombie WR, Gocayne JD, FitzGerald MG, Wallace S, Lee BM, Lamerdin J, Trapp S, Kelley JM, Liu LI (April 1992). "Automated DNA sequencing and analysis of 106 kilobases from human chromosome 19q13.3". Nature Genetics. 1 (1): 34–9. doi:10.1038/ng0492-34. PMID 1301997. S2CID 1986255.
- ^ Sabatakos G, Rowe GC, Kveiborg M, Wu M, Neff L, Chiusaroli R, Philbrick WM, Baron R (May 2008). "Doubly truncated FosB isoform (Delta2DeltaFosB) induces osteosclerosis in transgenic mice and modulates expression and phosphorylation of Smads in osteoblasts independent of intrinsic AP-1 activity". Journal of Bone and Mineral Research. 23 (5): 584–95. doi:10.1359/jbmr.080110. PMC 2674536. PMID 18433296.
- ^ a b c d e f g h i j k Ruffle JK (November 2014). "Molecular neurobiology of addiction: what's all the (Δ)FosB about?". The American Journal of Drug and Alcohol Abuse. 40 (6): 428–37. doi:10.3109/00952990.2014.933840. PMID 25083822. S2CID 19157711.
ΔFosB as a therapeutic biomarker
The strong correlation between chronic drug exposure and ΔFosB provides novel opportunities for targeted therapies in addiction (118), and suggests methods to analyze their efficacy (119). Over the past two decades, research has progressed from identifying ΔFosB induction to investigating its subsequent action (38). It is likely that ΔFosB research will now progress into a new era – the use of ΔFosB as a biomarker. If ΔFosB detection is indicative of chronic drug exposure (and is at least partly responsible for dependence of the substance), then its monitoring for therapeutic efficacy in interventional studies is a suitable biomarker (Figure 2). Examples of therapeutic avenues are discussed herein. ...
Conclusions
ΔFosB is an essential transcription factor implicated in the molecular and behavioral pathways of addiction following repeated drug exposure. The formation of ΔFosB in multiple brain regions, and the molecular pathway leading to the formation of AP-1 complexes is well understood. The establishment of a functional purpose for ΔFosB has allowed further determination as to some of the key aspects of its molecular cascades, involving effectors such as GluR2 (87,88), Cdk5 (93) and NFkB (100). Moreover, many of these molecular changes identified are now directly linked to the structural, physiological and behavioral changes observed following chronic drug exposure (60,95,97,102). New frontiers of research investigating the molecular roles of ΔFosB have been opened by epigenetic studies, and recent advances have illustrated the role of ΔFosB acting on DNA and histones, truly as a molecular switch (34). As a consequence of our improved understanding of ΔFosB in addiction, it is possible to evaluate the addictive potential of current medications (119), as well as use it as a biomarker for assessing the efficacy of therapeutic interventions (121,122,124). Some of these proposed interventions have limitations (125) or are in their infancy (75). However, it is hoped that some of these preliminary findings may lead to innovative treatments, which are much needed in addiction. - ^ a b c d e f g Nestler EJ (December 2013). "Cellular basis of memory for addiction". Dialogues in Clinical Neuroscience. 15 (4): 431–443. PMC 3898681. PMID 24459410.
Despite the importance of numerous psychosocial factors, at its core, drug addiction involves a biological process: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. ... A large body of literature has demonstrated that such ΔFosB induction in D1-type [nucleus accumbens] neurons increases an animal's sensitivity to drug as well as natural rewards and promotes drug self-administration, presumably through a process of positive reinforcement ... Another ΔFosB target is cFos: as ΔFosB accumulates with repeated drug exposure it represses c-Fos and contributes to the molecular switch whereby ΔFosB is selectively induced in the chronic drug-treated state.41 ... Moreover, there is increasing evidence that, despite a range of genetic risks for addiction across the population, exposure to sufficiently high doses of a drug for long periods of time can transform someone who has relatively lower genetic loading into an addict.
- ^ a b c Biliński P, Wojtyła A, Kapka-Skrzypczak L, Chwedorowicz R, Cyranka M, Studziński T (2012). "Epigenetic regulation in drug addiction". Annals of Agricultural and Environmental Medicine. 19 (3): 491–6. PMID 23020045.
For these reasons, ΔFosB is considered a primary and causative transcription factor in creating new neural connections in the reward centre, prefrontal cortex, and other regions of the limbic system. This is reflected in the increased, stable and long-lasting level of sensitivity to cocaine and other drugs, and tendency to relapse even after long periods of abstinence. These newly constructed networks function very efficiently via new pathways as soon as drugs of abuse are further taken ... In this way, the induction of CDK5 gene expression occurs together with suppression of the G9A gene coding for dimethyltransferase acting on the histone H3. A feedback mechanism can be observed in the regulation of these 2 crucial factors that determine the adaptive epigenetic response to cocaine. This depends on ΔFosB inhibiting G9a gene expression, i.e. H3K9me2 synthesis which in turn inhibits transcription factors for ΔFosB. For this reason, the observed hyper-expression of G9a, which ensures high levels of the dimethylated form of histone H3, eliminates the neuronal structural and plasticity effects caused by cocaine by means of this feedback which blocks ΔFosB transcription
- ^ Ohnishi YN, Ohnishi YH, Vialou V, Mouzon E, LaPlant Q, Nishi A, Nestler EJ (January 2015). "Functional role of the N-terminal domain of ΔFosB in response to stress and drugs of abuse". Neuroscience. 284: 165–70. doi:10.1016/j.neuroscience.2014.10.002. PMC 4268105. PMID 25313003.
- ^ Nakabeppu Y, Nathans D (February 1991). "A naturally occurring truncated form of FosB that inhibits Fos/Jun transcriptional activity". Cell. 64 (4): 751–9. doi:10.1016/0092-8674(91)90504-R. PMID 1900040. S2CID 23904956.
- ^ a b c Nestler EJ (October 2008). "Review. Transcriptional mechanisms of addiction: role of DeltaFosB". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 363 (1507): 3245–55. doi:10.1098/rstb.2008.0067. PMC 2607320. PMID 18640924.
Recent evidence has shown that ΔFosB also represses the c-fos gene that helps create the molecular switch—from the induction of several short-lived Fos family proteins after acute drug exposure to the predominant accumulation of ΔFosB after chronic drug exposure—cited earlier (Renthal et al. in press). The mechanism responsible for ΔFosB repression of c-fos expression is complex and is covered below. ...
Examples of validated targets for ΔFosB in nucleus accumbens ... GluR2 ... dynorphin ... Cdk5 ... NFκB ... c-Fos
Table 3 - ^ Renthal W, Nestler EJ (August 2008). "Epigenetic mechanisms in drug addiction". Trends in Molecular Medicine. 14 (8): 341–50. doi:10.1016/j.molmed.2008.06.004. PMC 2753378. PMID 18635399.
- ^ Renthal W, Kumar A, Xiao G, Wilkinson M, Covington HE, Maze I, Sikder D, Robison AJ, LaPlant Q, Dietz DM, Russo SJ, Vialou V, Chakravarty S, Kodadek TJ, Stack A, Kabbaj M, Nestler EJ (May 2009). "Genome-wide analysis of chromatin regulation by cocaine reveals a role for sirtuins". Neuron. 62 (3): 335–48. doi:10.1016/j.neuron.2009.03.026. PMC 2779727. PMID 19447090.
- ^ Sabatakos G, Sims NA, Chen J, Aoki K, Kelz MB, Amling M, Bouali Y, Mukhopadhyay K, Ford K, Nestler EJ, Baron R (September 2000). "Overexpression of DeltaFosB transcription factor(s) increases bone formation and inhibits adipogenesis". Nature Medicine. 6 (9): 985–90. doi:10.1038/79683. PMID 10973317. S2CID 20302360.
- ^ a b c d e Robison AJ, Nestler EJ (November 2011). "Transcriptional and epigenetic mechanisms of addiction". Nature Reviews Neuroscience. 12 (11): 623–637. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
ΔFosB serves as one of the master control proteins governing this structural plasticity. ... ΔFosB also represses G9a expression, leading to reduced repressive histone methylation at the cdk5 gene. The net result is gene activation and increased CDK5 expression. ... In contrast, ΔFosB binds to the c-fos gene and recruits several co-repressors, including HDAC1 (histone deacetylase 1) and SIRT 1 (sirtuin 1). ... The net result is c-fos gene repression.
Figure 4: Epigenetic basis of drug regulation of gene expression - ^ a b c d e Nestler EJ, Barrot M, Self DW (September 2001). "DeltaFosB: a sustained molecular switch for addiction". Proceedings of the National Academy of Sciences of the United States of America. 98 (20): 11042–6. Bibcode:2001PNAS...9811042N. doi:10.1073/pnas.191352698. PMC 58680. PMID 11572966.
- ^ Salaya-Velazquez NF, López-Muciño LA, Mejía-Chávez S, Sánchez-Aparicio P, Domínguez-Guadarrama AA, Venebra-Muñoz A (February 2020). "Anandamide and sucralose change ΔFosB expression in the reward system". NeuroReport. 31 (3): 240–244. doi:10.1097/WNR.0000000000001400. PMID 31923023. S2CID 210149592.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 364–375. ISBN 978-0-07-148127-4.
- ^ Volkow ND, Koob GF, McLellan AT (January 2016). "Neurobiologic Advances from the Brain Disease Model of Addiction". New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
Substance-use disorder: A diagnostic term in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) referring to recurrent use of alcohol or other drugs that causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. Depending on the level of severity, this disorder is classified as mild, moderate, or severe.
Addiction: A term used to indicate the most severe, chronic stage of substance-use disorder, in which there is a substantial loss of self-control, as indicated by compulsive drug taking despite the desire to stop taking the drug. In the DSM-5, the term addiction is synonymous with the classification of severe substance-use disorder. - ^ a b c Renthal W, Nestler EJ (September 2009). "Chromatin regulation in drug addiction and depression". Dialogues in Clinical Neuroscience. 11 (3): 257–268. doi:10.31887/DCNS.2009.11.3/wrenthal. PMC 2834246. PMID 19877494.
[Psychostimulants] increase cAMP levels in striatum, which activates protein kinase A (PKA) and leads to phosphorylation of its targets. This includes the cAMP response element binding protein (CREB), the phosphorylation of which induces its association with the histone acetyltransferase, CREB binding protein (CBP) to acetylate histones and facilitate gene activation. This is known to occur on many genes including fosB and c-fos in response to psychostimulant exposure. ΔFosB is also upregulated by chronic psychostimulant treatments, and is known to activate certain genes (eg, cdk5) and repress others (eg, c-fos) where it recruits HDAC1 as a corepressor. ... Chronic exposure to psychostimulants increases glutamatergic [signaling] from the prefrontal cortex to the NAc. Glutamatergic signaling elevates Ca2+ levels in NAc postsynaptic elements where it activates CaMK (calcium/calmodulin protein kinases) signaling, which, in addition to phosphorylating CREB, also phosphorylates HDAC5.
Figure 2: Psychostimulant-induced signaling events - ^ Broussard JI (January 2012). "Co-transmission of dopamine and glutamate". The Journal of General Physiology. 139 (1): 93–96. doi:10.1085/jgp.201110659. PMC 3250102. PMID 22200950.
Coincident and convergent input often induces plasticity on a postsynaptic neuron. The NAc integrates processed information about the environment from basolateral amygdala, hippocampus, and prefrontal cortex (PFC), as well as projections from midbrain dopamine neurons. Previous studies have demonstrated how dopamine modulates this integrative process. For example, high frequency stimulation potentiates hippocampal inputs to the NAc while simultaneously depressing PFC synapses (Goto and Grace, 2005). The converse was also shown to be true; stimulation at PFC potentiates PFC–NAc synapses but depresses hippocampal–NAc synapses. In light of the new functional evidence of midbrain dopamine/glutamate co-transmission (references above), new experiments of NAc function will have to test whether midbrain glutamatergic inputs bias or filter either limbic or cortical inputs to guide goal-directed behavior.
- ^ Kanehisa Laboratories (10 October 2014). "Amphetamine – Homo sapiens (human)". KEGG Pathway. Retrieved 31 October 2014.
Most addictive drugs increase extracellular concentrations of dopamine (DA) in nucleus accumbens (NAc) and medial prefrontal cortex (mPFC), projection areas of mesocorticolimbic DA neurons and key components of the "brain reward circuit". Amphetamine achieves this elevation in extracellular levels of DA by promoting efflux from synaptic terminals. ... Chronic exposure to amphetamine induces a unique transcription factor delta FosB, which plays an essential role in long-term adaptive changes in the brain.
- ^ Cadet JL, Brannock C, Jayanthi S, Krasnova IN (2015). "Transcriptional and epigenetic substrates of methamphetamine addiction and withdrawal: evidence from a long-access self-administration model in the rat". Molecular Neurobiology. 51 (2): 696–717 (Figure 1). doi:10.1007/s12035-014-8776-8. PMC 4359351. PMID 24939695.
- ^ a b c d Nestler EJ (December 2012). "Transcriptional mechanisms of drug addiction". Clinical Psychopharmacology and Neuroscience. 10 (3): 136–143. doi:10.9758/cpn.2012.10.3.136. PMC 3569166. PMID 23430970.
The 35-37 kD ΔFosB isoforms accumulate with chronic drug exposure due to their extraordinarily long half-lives. ... As a result of its stability, the ΔFosB protein persists in neurons for at least several weeks after cessation of drug exposure. ... ΔFosB overexpression in nucleus accumbens induces NFκB ... In contrast, the ability of ΔFosB to repress the c-Fos gene occurs in concert with the recruitment of a histone deacetylase and presumably several other repressive proteins such as a repressive histone methyltransferase
- ^ Nestler EJ (October 2008). "Transcriptional mechanisms of addiction: Role of ΔFosB". Philosophical Transactions of the Royal Society B: Biological Sciences. 363 (1507): 3245–3255. doi:10.1098/rstb.2008.0067. PMC 2607320. PMID 18640924.
Recent evidence has shown that ΔFosB also represses the c-fos gene that helps create the molecular switch—from the induction of several short-lived Fos family proteins after acute drug exposure to the predominant accumulation of ΔFosB after chronic drug exposure
- ^ a b Hyman SE, Malenka RC, Nestler EJ (2006). "Neural mechanisms of addiction: the role of reward-related learning and memory". Annual Review of Neuroscience. 29: 565–98. doi:10.1146/annurev.neuro.29.051605.113009. PMID 16776597.
- ^ Steiner H, Van Waes V (January 2013). "Addiction-related gene regulation: risks of exposure to cognitive enhancers vs. other psychostimulants". Progress in Neurobiology. 100: 60–80. doi:10.1016/j.pneurobio.2012.10.001. PMC 3525776. PMID 23085425.
- ^ Kim Y, Teylan MA, Baron M, Sands A, Nairn AC, Greengard P (February 2009). "Methylphenidate-induced dendritic spine formation and DeltaFosB expression in nucleus accumbens". Proceedings of the National Academy of Sciences of the United States of America. 106 (8): 2915–20. Bibcode:2009PNAS..106.2915K. doi:10.1073/pnas.0813179106. PMC 2650365. PMID 19202072.
- ^ a b c d Nestler EJ (January 2014). "Epigenetic mechanisms of drug addiction". Neuropharmacology. 76 Pt B: 259–268. doi:10.1016/j.neuropharm.2013.04.004. PMC 3766384. PMID 23643695.
Short-term increases in histone acetylation generally promote behavioral responses to the drugs, while sustained increases oppose cocaine's effects, based on the actions of systemic or intra-NAc administration of HDAC inhibitors. ... Genetic or pharmacological blockade of G9a in the NAc potentiates behavioral responses to cocaine and opiates, whereas increasing G9a function exerts the opposite effect (Maze et al., 2010; Sun et al., 2012a). Such drug-induced downregulation of G9a and H3K9me2 also sensitizes animals to the deleterious effects of subsequent chronic stress (Covington et al., 2011). Downregulation of G9a increases the dendritic arborization of NAc neurons, and is associated with increased expression of numerous proteins implicated in synaptic function, which directly connects altered G9a/H3K9me2 in the synaptic plasticity associated with addiction (Maze et al., 2010).
G9a appears to be a critical control point for epigenetic regulation in NAc, as we know it functions in two negative feedback loops. It opposes the induction of ΔFosB, a long-lasting transcription factor important for drug addiction (Robison and Nestler, 2011), while ΔFosB in turn suppresses G9a expression (Maze et al., 2010; Sun et al., 2012a). ... Also, G9a is induced in NAc upon prolonged HDAC inhibition, which explains the paradoxical attenuation of cocaine's behavioral effects seen under these conditions, as noted above (Kennedy et al., 2013). GABAA receptor subunit genes are among those that are controlled by this feedback loop. Thus, chronic cocaine, or prolonged HDAC inhibition, induces several GABAA receptor subunits in NAc, which is associated with increased frequency of inhibitory postsynaptic currents (IPSCs). In striking contrast, combined exposure to cocaine and HDAC inhibition, which triggers the induction of G9a and increased global levels of H3K9me2, leads to blockade of GABAA receptor and IPSC regulation. - ^ a b McCowan TJ, Dhasarathy A, Carvelli L (February 2015). "The Epigenetic Mechanisms of Amphetamine". J. Addict. Prev. 2015 (Suppl 1). PMC 4955852. PMID 27453897.
Epigenetic modifications caused by addictive drugs play an important role in neuronal plasticity and in drug-induced behavioral responses. Although few studies have investigated the effects of AMPH on gene regulation (Table 1), current data suggest that AMPH acts at multiple levels to alter histone/DNA interaction and to recruit transcription factors which ultimately cause repression of some genes and activation of other genes. Importantly, some studies have also correlated the epigenetic regulation induced by AMPH with the behavioral outcomes caused by this drug, suggesting therefore that epigenetics remodeling underlies the behavioral changes induced by AMPH. If this proves to be true, the use of specific drugs that inhibit histone acetylation, methylation or DNA methylation might be an important therapeutic alternative to prevent and/or reverse AMPH addiction and mitigate the side effects generate by AMPH when used to treat ADHD.
- ^ a b c d Walker DM, Cates HM, Heller EA, Nestler EJ (February 2015). "Regulation of chromatin states by drugs of abuse". Curr. Opin. Neurobiol. 30: 112–121. doi:10.1016/j.conb.2014.11.002. PMC 4293340. PMID 25486626.
Studies investigating general HDAC inhibition on behavioral outcomes have produced varying results but it seems that the effects are specific to the timing of exposure (either before, during or after exposure to drugs of abuse) as well as the length of exposure
- ^ a b Primary references involving sodium butyrate:
• Kennedy PJ, Feng J, Robison AJ, Maze I, Badimon A, Mouzon E, Chaudhury D, Damez-Werno DM, Haggarty SJ, Han MH, Bassel-Duby R, Olson EN, Nestler EJ (April 2013). "Class I HDAC inhibition blocks cocaine-induced plasticity by targeted changes in histone methylation". Nat. Neurosci. 16 (4): 434–440. doi:10.1038/nn.3354. PMC 3609040. PMID 23475113.While acute HDAC inhibition enhances the behavioral effects of cocaine or amphetamine1,3,4,13,14, studies suggest that more chronic regimens block psychostimulant-induced plasticity3,5,11,12. ... The effects of pharmacological inhibition of HDACs on psychostimulant-induced plasticity appear to depend on the timecourse of HDAC inhibition. Studies employing co-administration procedures in which inhibitors are given acutely, just prior to psychostimulant administration, report heightened behavioral responses to the drug1,3,4,13,14. In contrast, experimental paradigms like the one employed here, in which HDAC inhibitors are administered more chronically, for several days prior to psychostimulant exposure, show inhibited expression3 or decreased acquisition of behavioral adaptations to drug5,11,12. The clustering of seemingly discrepant results based on experimental methodologies is interesting in light of our present findings. Both HDAC inhibitors and psychostimulants increase global levels of histone acetylation in NAc. Thus, when co-administered acutely, these drugs may have synergistic effects, leading to heightened transcriptional activation of psychostimulant-regulated target genes. In contrast, when a psychostimulant is given in the context of prolonged, HDAC inhibitor-induced hyperacetylation, homeostatic processes may direct AcH3 binding to the promoters of genes (e.g., G9a) responsible for inducing chromatin condensation and gene repression (e.g., via H3K9me2) in order to dampen already heightened transcriptional activation. Our present findings thus demonstrate clear cross talk among histone PTMs and suggest that decreased behavioral sensitivity to psychostimulants following prolonged HDAC inhibition might be mediated through decreased activity of HDAC1 at H3K9 KMT promoters and subsequent increases in H3K9me2 and gene repression.
• Simon-O'Brien E, Alaux-Cantin S, Warnault V, Buttolo R, Naassila M, Vilpoux C (July 2015). "The histone deacetylase inhibitor sodium butyrate decreases excessive ethanol intake in dependent animals". Addict Biol. 20 (4): 676–689. doi:10.1111/adb.12161. PMID 25041570. S2CID 28667144.Altogether, our results clearly demonstrated the efficacy of NaB in preventing excessive ethanol intake and relapse and support the hypothesis that HDACi may have a potential use in alcohol addiction treatment.
• Castino MR, Cornish JL, Clemens KJ (April 2015). "Inhibition of histone deacetylases facilitates extinction and attenuates reinstatement of nicotine self-administration in rats". PLOS ONE. 10 (4): e0124796. Bibcode:2015PLoSO..1024796C. doi:10.1371/journal.pone.0124796. PMC 4399837. PMID 25880762.treatment with NaB significantly attenuated nicotine and nicotine + cue reinstatement when administered immediately ... These results provide the first demonstration that HDAC inhibition facilitates the extinction of responding for an intravenously self-administered drug of abuse and further highlight the potential of HDAC inhibitors in the treatment of drug addiction.
- ^ Kyzar EJ, Pandey SC (August 2015). "Molecular mechanisms of synaptic remodeling in alcoholism". Neurosci. Lett. 601: 11–9. doi:10.1016/j.neulet.2015.01.051. PMC 4506731. PMID 25623036.
Increased HDAC2 expression decreases the expression of genes important for the maintenance of dendritic spine density such as BDNF, Arc, and NPY, leading to increased anxiety and alcohol-seeking behavior. Decreasing HDAC2 reverses both the molecular and behavioral consequences of alcohol addiction, thus implicating this enzyme as a potential treatment target (Fig. 3). HDAC2 is also crucial for the induction and maintenance of structural synaptic plasticity in other neurological domains such as memory formation [115]. Taken together, these findings underscore the potential usefulness of HDAC inhibition in treating alcohol use disorders ... Given the ability of HDAC inhibitors to potently modulate the synaptic plasticity of learning and memory [118], these drugs hold potential as treatment for substance abuse-related disorders. ... Our lab and others have published extensively on the ability of HDAC inhibitors to reverse the gene expression deficits caused by multiple models of alcoholism and alcohol abuse, the results of which were discussed above [25,112,113]. This data supports further examination of histone modifying agents as potential therapeutic drugs in the treatment of alcohol addiction ... Future studies should continue to elucidate the specific epigenetic mechanisms underlying compulsive alcohol use and alcoholism, as this is likely to provide new molecular targets for clinical intervention.
- ^ Kheirabadi GR, Ghavami M, Maracy MR, Salehi M, Sharbafchi MR (2016). "Effect of add-on valproate on craving in methamphetamine depended patients: A randomized trial". Advanced Biomedical Research. 5: 149. doi:10.4103/2277-9175.187404. PMC 5025910. PMID 27656618.
- ^ Hope BT (May 1998). "Cocaine and the AP-1 transcription factor complex". Annals of the New York Academy of Sciences. 844 (1): 1–6. Bibcode:1998NYASA.844....1H. doi:10.1111/j.1749-6632.1998.tb08216.x. PMID 9668659. S2CID 11683570.
- ^ a b Kelz MB, Chen J, Carlezon WA, Whisler K, Gilden L, Beckmann AM, Steffen C, Zhang YJ, Marotti L, Self DW, Tkatch T, Baranauskas G, Surmeier DJ, Neve RL, Duman RS, Picciotto MR, Nestler EJ (September 1999). "Expression of the transcription factor deltaFosB in the brain controls sensitivity to cocaine". Nature. 401 (6750): 272–6. Bibcode:1999Natur.401..272K. doi:10.1038/45790. PMID 10499584. S2CID 4390717.
- ^ a b Colby CR, Whisler K, Steffen C, Nestler EJ, Self DW (March 2003). "Striatal cell type-specific overexpression of DeltaFosB enhances incentive for cocaine". The Journal of Neuroscience. 23 (6): 2488–93. doi:10.1523/JNEUROSCI.23-06-02488.2003. PMC 6742034. PMID 12657709.
- ^ Cao X, Yasuda T, Uthayathas S, Watts RL, Mouradian MM, Mochizuki H, Papa SM (May 2010). "Striatal overexpression of DeltaFosB reproduces chronic levodopa-induced involuntary movements". The Journal of Neuroscience. 30 (21): 7335–43. doi:10.1523/JNEUROSCI.0252-10.2010. PMC 2888489. PMID 20505100.
- ^ a b c d e Du H, Nie S, Chen G, Ma K, Xu Y, Zhang Z, Papa SM, Cao X (2015). "Levetiracetam Ameliorates L-DOPA-Induced Dyskinesia in Hemiparkinsonian Rats Inducing Critical Molecular Changes in the Striatum". Parkinson's Disease. 2015: 253878. doi:10.1155/2015/253878. PMC 4322303. PMID 25692070.
Furthermore, the transgenic overexpression of ΔFosB reproduces AIMs in hemiparkinsonian rats without chronic exposure to L-DOPA [13]. ... FosB/ΔFosB immunoreactive neurons increased in the dorsolateral part of the striatum on the lesion side with the used antibody that recognizes all members of the FosB family. All doses of levetiracetam decreased the number of FosB/ΔFosB positive cells (from 88.7 ± 1.7/section in the control group to 65.7 ± 0.87, 42.3 ± 1.88, and 25.7 ± 1.2/section in the 15, 30, and 60 mg groups, resp.; Figure 2). These results indicate dose-dependent effects of levetiracetam on FosB/ΔFosB expression. ... In addition, transcription factors expressed with chronic events such as ΔFosB (a truncated splice variant of FosB) are overexpressed in the striatum of rodents and primates with dyskinesias [9, 10]. ... Furthermore, ΔFosB overexpression has been observed in postmortem striatal studies of Parkinsonian patients chronically treated with L-DOPA [26]. ... Of note, the most prominent effect of levetiracetam was the reduction of ΔFosB expression, which cannot be explained by any of its known actions on vesicular protein or ion channels. Therefore, the exact mechanism(s) underlying the antiepileptic effects of levetiracetam remains uncertain.
- ^ "ROLE OF ΔFOSB IN THE NUCLEUS ACCUMBENS". Mount Sinai School of Medicine. NESTLER LAB: LABORATORY OF MOLECULAR PSYCHIATRY. Archived from the original on 28 June 2017. Retrieved 6 September 2014.
- ^ Furuyashiki T, Deguchi Y (August 2012). "[Roles of altered striatal function in major depression]". Brain and Nerve = Shinkei Kenkyū No Shinpo (in Japanese). 64 (8): 919–26. PMID 22868883.
- ^ Nestler EJ (April 2015). "∆FosB: a transcriptional regulator of stress and antidepressant responses". European Journal of Pharmacology. 753: 66–72. doi:10.1016/j.ejphar.2014.10.034. PMC 4380559. PMID 25446562.
In more recent years, prolonged induction of ∆FosB has also been observed within NAc in response to chronic administration of certain forms of stress. Increasing evidence indicates that this induction represents a positive, homeostatic adaptation to chronic stress, since overexpression of ∆FosB in this brain region promotes resilience to stress, whereas blockade of its activity promotes stress susceptibility. Chronic administration of several antidepressant medications also induces ∆FosB in the NAc, and this induction is required for the therapeutic-like actions of these drugs in mouse models. Validation of these rodent findings is the demonstration that depressed humans, examined at autopsy, display reduced levels of ∆FosB within the NAc. As a transcription factor, ΔFosB produces this behavioral phenotype by regulating the expression of specific target genes, which are under current investigation. These studies of ΔFosB are providing new insight into the molecular basis of depression and antidepressant action, which is defining a host of new targets for possible therapeutic development.
- ^ Dietz DM, Kennedy PJ, Sun H, Maze I, Gancarz AM, Vialou V, Koo JW, Mouzon E, Ghose S, Tamminga CA, Nestler EJ (February 2014). "ΔFosB induction in prefrontal cortex by antipsychotic drugs is associated with negative behavioral outcomes". Neuropsychopharmacology. 39 (3): 538–44. doi:10.1038/npp.2013.255. PMC 3895248. PMID 24067299.
Further reading
- Schuermann M, Jooss K, Müller R (April 1991). "fosB is a transforming gene encoding a transcriptional activator". Oncogene. 6 (4): 567–76. PMID 1903195.
- Brown JR, Ye H, Bronson RT, Dikkes P, Greenberg ME (July 1996). "A defect in nurturing in mice lacking the immediate early gene fosB". Cell. 86 (2): 297–309. doi:10.1016/S0092-8674(00)80101-4. PMID 8706134. S2CID 17266171.
- Heximer SP, Cristillo AD, Russell L, Forsdyke DR (December 1996). "Sequence analysis and expression in cultured lymphocytes of the human FOSB gene (G0S3)". DNA and Cell Biology. 15 (12): 1025–38. doi:10.1089/dna.1996.15.1025. PMID 8985116.
- Liberati NT, Datto MB, Frederick JP, Shen X, Wong C, Rougier-Chapman EM, Wang XF (April 1999). "Smads bind directly to the Jun family of AP-1 transcription factors". Proceedings of the National Academy of Sciences of the United States of America. 96 (9): 4844–9. Bibcode:1999PNAS...96.4844L. doi:10.1073/pnas.96.9.4844. PMC 21779. PMID 10220381.
- Yamamura Y, Hua X, Bergelson S, Lodish HF (November 2000). "Critical role of Smads and AP-1 complex in transforming growth factor-beta -dependent apoptosis". The Journal of Biological Chemistry. 275 (46): 36295–302. doi:10.1074/jbc.M006023200. PMID 10942775.
- Bergman MR, Cheng S, Honbo N, Piacentini L, Karliner JS, Lovett DH (February 2003). "A functional activating protein 1 (AP-1) site regulates matrix metalloproteinase 2 (MMP-2) transcription by cardiac cells through interactions with JunB-Fra1 and JunB-FosB heterodimers". Biochemical Journal. 369 (Pt 3): 485–96. doi:10.1042/BJ20020707. PMC 1223099. PMID 12371906.
- Milde-Langosch K, Kappes H, Riethdorf S, Löning T, Bamberger AM (February 2003). "FosB is highly expressed in normal mammary epithelia, but down-regulated in poorly differentiated breast carcinomas". Breast Cancer Research and Treatment. 77 (3): 265–75. doi:10.1023/A:1021887100216. PMID 12602926. S2CID 987857.
- Baumann S, Hess J, Eichhorst ST, Krueger A, Angel P, Krammer PH, Kirchhoff S (March 2003). "An unexpected role for FosB in activation-induced cell death of T cells". Oncogene. 22 (9): 1333–9. doi:10.1038/sj.onc.1206126. PMID 12618758. S2CID 10696422.
- Holmes DI, Zachary I (January 2004). "Placental growth factor induces FosB and c-Fos gene expression via Flt-1 receptors". FEBS Letters. 557 (1–3): 93–8. doi:10.1016/S0014-5793(03)01452-2. PMID 14741347. S2CID 6596900.
- Konsman JP, Blomqvist A (May 2005). "Forebrain patterns of c-Fos and FosB induction during cancer-associated anorexia-cachexia in rat". The European Journal of Neuroscience. 21 (10): 2752–66. doi:10.1111/j.1460-9568.2005.04102.x. PMID 15926923. S2CID 40045788.
External links
- ROLE OF ΔFOSB IN THE NUCLEUS ACCUMBENS Archived 28 June 2017 at the Wayback Machine
- KEGG Pathway – human alcohol addiction
- KEGG Pathway – human amphetamine addiction
- KEGG Pathway – human cocaine addiction
- FOSB+protein,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
This article incorporates text from the United States National Library of Medicine, which is in the public domain.
Diagnosis
DSM
The American Psychiatric Association publishes and periodically updates the Diagnostic and Statistical Manual of Mental Disorders (DSM), a widely recognized compendium of mental health diagnostics.[1]
The version published in 1987 (DSM-III-R), referred to "distress about a pattern of repeated sexual conquests or other forms of nonparaphilic sexual addiction, involving a succession of people who exist only as things to be used."[2] The reference to sexual addiction was subsequently removed.[3] The DSM-IV-TR, published in 2000 (DSM-IV-TR), did not include sexual addiction as a mental disorder.[4] The DSM-IV-TR included a miscellaneous diagnosis called Sexual Disorders Not Otherwise Specified, stating : "distress about a pattern of repeated sexual relationships involving a succession of lovers who are experienced by the individual only as things to be used." (Other examples include: compulsive fixation on an unattainable partner, compulsive masturbation, compulsive love relationships, and compulsive sexuality in a relationship.)[4]
Some authors suggested that sexual addiction should be re-introduced into the DSM system;[5] however, sexual addiction was rejected for inclusion in the DSM-5, which was published in 2013.[6] Darrel Regier, vice-chair of the DSM-5 task force, said that "[A]lthough 'hypersexuality' is a proposed new addition...[the phenomenon] was not at the point where we were ready to call it an addiction." The proposed diagnosis does not make the cut as an official diagnosis due to a lack of research into diagnostic criteria for compulsive sexual behavior, according to the American Psychiatric Association.[7][8]
Borderline personality disorder
The American Psychiatric Association uses the Diagnostic and Statistical Manual of Mental Disorders (DSM) to define and classify mental illnesses and in the DSM-IV version of the document, it lists borderline personality disorder (BPD) as an Axis II – Cluster B personality disorder with the code 301.83. The DSM-5 dropped the multiaxial system, but BPD still retains the same numerical code of 301.83.[7] The World Health Organization's produces the International Classification of Diseases (ICD) and lists BPD under the name "Emotionally unstable personality disorder". The latest version of the document (ICD-10) lists the disorder in Chapter X which is reserved for "Disorders of adult personality and behaviour" and has the code F60.3.[9] The Chinese Society of Psychiatry uses the Chinese Classification of Mental Disorders (CCMD), which is in its third edition (CCMD-3) and has a diagnosis of "Nonorganic sexual dysfunction" (numerical code 52.9), of which sexual promiscuity may be a symptom. Personality disorders, Habit and impulse disorders, Psychosexual disorders in the CCMD-3 fall in Chapter 6 and under code 6.60 are listed the personality disorders. The CCMD-3 lists "impulsive personality disorder" (numerical code 60.4),[10] which is equivalent to what the DSM refers to as "borderline personality disorder" and what the ICD-10 refers to as "emotionally unstable personality disorder". All three classification manuals and documents list sexual promiscuity as a prevalent and problematic symptom for patients with this particular pathology. Hypersexuality along with high-risk sexual behaviour, seductive behaviour, and promiscuity are an often due to the marked impulsivity common to this group of patients. Individuals with borderline personality disorder (emotionally unstable personality disorder or impulsive personality disorder) not only are prone to promiscuity, but in many cases, co-morbid paraphilias and fetishistic behaviour are commonly associated with their sexual behaviours. Common paraphilic compulsions among individuals with this diagnosis include urolagnia ("golden showers"), sadomasochism, voyeurism, autassassinophilia, partialism, biastophilia, and in some cases paraphilic drives may be more extreme and dangerous – such as erotophonophilia, necrophilia, pedophilia, and even anthropophagy. Both males and females with this personality disorder often have a strong desire and compulsion to get involved in illicit sex, affairs, and relationships with married or otherwise pre-attached individuals. Consequently, individuals with borderline personality disorder often experience love and sexuality in perverse and violent qualities which they cannot integrate with the tender, intimate side of relationships.[11][12]
ICD
The World Health Organization produces the International Classification of Diseases (ICD), which is not limited to mental disorders. The most recent version of that document, ICD-10, includes "Excessive sexual drive" as a diagnosis (code F52.8), subdividing it into satyriasis (for males) and nymphomania (for females).[13]
CCMD
The Chinese Society of Psychiatry produces the Chinese Classification of Mental Disorders (CCMD), which is currently in its third edition – the CCMD-3 and Chapter 5 of the document lists "Physiological disorders related to psychological factors" and under code 52 are disorders that are "Nonorganic sexual dysfuction," and within that category are listed a number of disorders, one of which is "Other or unspecified sexual dysfunction" (numerical code 52.9).[14] This is roughly equivalent to the ICD-10 diagnosis of "Other sexual dysfunction not due to a substance or known physiological condition" (specifier Excessive sexual drive) (F52.8) and "Unspecified sexual dysfunction not due to a substance or known physiological condition" (F52.9).[15]
Diagnostic criteria
Several mental health providers have proposed various, but similar, criteria for diagnosing sexual addiction, including Patrick Carnes,[16] and Aviel Goodman.[17] Dr. Carnes authored the first clinical book about sex addiction in 1983 based on his own empirical research. His diagnostic model is still largely utilized by the thousands of certified sex addiction therapists (CSATs) trained by the organization he founded.[18] No diagnostic proposal for sex addiction has been adopted into any official government diagnostic manual, however.
During the update of the Diagnostic and Statistical Manual to version 5 (DSM-5), the American Psychiatric Association rejected two independent proposals for inclusion.[citation needed]
The International Classification of Diseases (ICD-10) of the World Health Organization, however, does include an entry for "Excessive Masturbation"[19] and another for "Excessive Sexual Drive."[20]
In 2011, the American Society of Addiction Medicine (ASAM), the largest medical consensus of physicians dedicated to treating and preventing addiction,[21] redefined addiction as a chronic brain disorder[22] which for the first time broadened the definition of addiction from substances to include addictive behaviors and reward-seeking, such as gambling and sex.[23]
Treatment
This section needs more reliable medical references for verification or relies too heavily on primary sources. (June 2015) |  |
Behavioral therapy
Cognitive behavioral therapy is a common form of behavioral treatment for addictions and maladaptive behaviors in general.
This article needs additional citations for verification. (October 2014) |
Dialectical behavior therapy has been shown to improve treatment outcomes as well. Certified Sex Addiction Therapists (CSAT) – a group of sexual addiction therapists certified by the International Institute for Trauma and Addiction Professionals – offer specialized behavioral therapy designed specifically for sexual addiction.[18][24]
Intensive outpatient programs for sexual addiction provide intensive treatment for individuals over the course of several weeks or months. An intensive outpatient program can help stabilize an individual who may be in crisis, but may not need inpatient treatment. Individuals who successfully complete an intensive outpatient program may then continue with less frequent treatment services such as individual counseling, group counseling, and couples counseling to help continue work toward and maintenance of their recovery. Intensive outpatient programs can help clients address, understand and overcome triggers in their everyday lives that may be contributing to compulsive sexual behavior and acting out.
Twelve-step programs
Involvement in twelve-step programs for sex addiction can also serve as an adjunct therapy to supplement clinical treatment. Self-help groups exist in most of the developed world. Such programs include Sexaholics Anonymous, Sex Addicts Anonymous, Sex and Love Addicts Anonymous, Celebrate Recovery, and others.
Epidemiology
According to a systematic review from 2014, prevalence rates of sexual addiction and related sexual disorders ranges from 3% to 6%.[25]
History
Sex addiction as a term first emerged in the mid-1970s when various members of Alcoholics Anonymous sought to apply the principles of 12-Steps toward sexual recovery from serial infidelity and other unmanageable compulsive sex behaviors that were similar to the powerlessness and un-manageability they experienced with alcoholism.[26] Multiple 12-step style self-help groups now exist for people who identify as sex addicts, including Sex Addicts Anonymous, Sexaholics Anonymous, Sex and Love Addicts Anonymous, and Sexual Compulsives Anonymous.
Society and culture
Controversy
| External media | |
|---|---|
| Images | |
| Audio | |
| Video | |
The controversy surrounding sexual addiction is centered around its identification, through a diagnostic model, in a clinical setting. As noted in current medical literature reviews, compulsive sexual behavior has been observed in humans;[27][28] drug-induced compulsive sexual behavior has also been noted clinically in some individuals taking dopaminergic drugs.[27] Moreover, current medical research involving neuropsychological models has identified sexual addictions (i.e., the compulsive engagement in sexual behavior despite negative consequences) as a true form of addiction (i.e., it possesses all the necessary characteristics to classify it as one) in animal models.[27][28] Since current diagnostic models use drug-related concepts as diagnostic criteria for addictions,[1] these are ill-suited for modelling compulsive behaviors in a clinical setting.[27] Consequently, diagnostic classification systems, such as the DSM, do not include sexual addiction as a diagnosis because there is currently "insufficient peer-reviewed evidence to establish the diagnostic criteria and course descriptions needed to identify these behaviors as mental disorders".[7] A 2014 systematic review on sexual addiction indicated that the "lack of empirical evidence on sexual addiction is the result of the disease's complete absence from versions of the Diagnostic and Statistical Manual of Mental Disorders."[25]
There have been debates regarding the definition and existence of sexual addictions for decades, as the issue was covered in a 1994 journal article.[29][30] According to a 2014 systematic review, sexual addiction (including excessive masturbation and pornography addiction) a diagnosable behavioral addiction with estimable prevalence rates.[25] The Mayo Clinic considers sexual addiction to be a form of obsessive compulsive disorder and refer to it as sexual compulsivity (note that by definition, an addiction is a compulsion toward rewarding stimuli).[31] A paper dating back to 1988 and a journal comment letter published in 2006 asserted that sex addiction is itself a myth, a by-product of cultural and other influences.[32][33] The 1988 paper argued that the condition is instead a way of projecting social stigma onto patients.[32]
In a non-academic opinion report from 2003, Marty Klein, stated that "the concept of sex addiction provides an excellent example of a model that is both sex-negative and politically disastrous."[34]: 8 Klein singled out a number of features that he considered crucial limitations of the sex addiction model[34]: 8 and stated that the diagnostic criteria for sexual addiction are easy to find on the internet.[34]: 9 Drawing on the Sexual Addiction Screening Test, he stated that "the sexual addiction diagnostic criteria make problems of nonproblematic experiences, and as a result pathologize a majority of people."[34]: 10
Popular culture
Sexual addiction has been the main theme in films such as 2001 film Diary of a Sex Addict, 2005 film I Am a Sex Addict, 2006 film Black Snake Moan, 2008 film Confessions of a Porn Addict, 2011 film Shame, 2012 film Thanks for Sharing, and others.
In Buddhism
In the Kama Sutta from the Sutta Nipata the Buddha explains that craving and attachment to sexual pleasure is a cause of suffering:
If one, longing for sexual pleasure, achieves it, yes, he's enraptured at heart. The mortal gets what he wants. But if for that person — longing, desiring — the pleasures diminish, he's shattered, as if shot with an arrow.
— Kama Sutta, Sutta Nipata[35]
The Buddha then goes on to say:
So one, always mindful, should avoid sexual desires. Letting them go, he will cross over the flood like one who, having bailed out the boat, has reached the far shore.
See also
- Compulsive masturbation
- Hypersexuality
- Pornography addiction
- Internet sex addiction
- Sexual obsessions
References
- ^ a b Cite error: The named reference
NHM terms-DSM flawwas invoked but never defined (see the help page). - ^ American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., rev.). Washington, DC: Author.
- ^ Kafka, M. P. (2010). "Hypersexual Disorder: A proposed diagnosis for DSM-V" (PDF). Archives of Sexual Behavior. 39 (2): 377–400. doi:10.1007/s10508-009-9574-7. PMID 19937105.
- ^ a b American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (fourth edition, text revision). Washington, DC: Author.
- ^ Irons, R.; Irons, J. P. (1996). "Differential diagnosis of addictive sexual disorders using the DSM-IV". Sexual Addiction & Compulsivity. 3: 7–21. doi:10.1080/10720169608400096.
- ^ Psychiatry's bible: Autism, binge-eating updates proposed for 'DSM' USA Today.
- ^ a b c American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (Fifth ed.). Arlington, VA: American Psychiatric Publishing. pp. 481, 797–798. ISBN 978-0-89042-555-8.
Thus, groups of repetitive behaviors, which some term behavioral addictions, with such subcategories as "sex addiction," "exercise addiction," or "shopping addiction," are not included because at this time there is insufficient peer-reviewed evidence to establish the diagnostic criteria and course descriptions needed to identify these behaviors as mental disorders.
- ^ Rachael Rettner (6 December 2012). "'Sex Addiction' Still Not Official Disorder". LiveScience. Retrieved 2 January 2013.
- ^ "International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) Version for 2010". International Statistical Classification of Diseases and Related Health Problems. World Health Organization. Retrieved 3 July 2014.
- ^ "CCMD-3". Chinese Society of Psychiatry. Chinese Classification of Mental Disorders (third edition). Retrieved 3 July 2014.
- ^ Mitchell, Stephen (1995). Freud and Beyond: A History of Modern Psychoanalytic Thought. New York: Basic Books. ISBN 978-0-465-01405-7.
- ^ Hull J. W.; Clarkin J. F.; Yeomans F. (1993). "Borderline personality disorder and impulsive sexual behavior". Psychiatric Services. 44 (10): 1000–1001. doi:10.1176/ps.44.10.1000.
- ^ International Classification of Diseases Expert Coding Manual for Physicians, 2016 update.
- ^ "Chinese Society of Psychiatry". Chinese Classification of Mental Disorders (CCMD). Ministry of Health. Retrieved 3 July 2014.
- ^ "ICD-10-CM – 2016 update". Retrieved 2 March 2016.
- ^ Patrick Carnes; David Delmonico; Elizabeth Griffin (2001). In the Shadows of the Net. p. 31. ISBN 1-59285-149-5.
- ^ Goodman, Aviel (1998). Sexual Addiction: An Integrated Approach. Madison, Connecticut: International Universities Press. pp. 233–234. ISBN 978-0-8236-6063-6Template:Inconsistent citations
{{cite book}}: CS1 maint: postscript (link) - ^ a b IITAP Official Website
- ^ "2012 ICD-10-CM Diagnosis Code F98.8 : Other specified behavioral and emotional disorders with onset usually occurring in childhood and adolescence". Icd10data.com. Retrieved 22 June 2012.
- ^ "2012 ICD-10 Diagnosis Code F52.7 : Excessive sexual drive". Retrieved 22 February 2013.
- ^ "2011 New definition of addiction: Addiction is a chronic brain disease, not just bad behavior or bad choices". Retrieved 15 August 2011.
- ^ "2011 Addiction Now Defined As Brain Disorder, Not Behavior Issue". Retrieved 15 August 2011.
- ^ "2011 ASAM: The Definition of Addiction". Retrieved 12 April 2011.
- ^ Stefanie Carnes. Mending a Shattered Heart: A Guide for Partners of Sex Addicts. Gentle Path Press; Second Edition. (4 October 2011) page 139 ISBN 978-0-9826505-9-2
- ^ a b c Cite error: The named reference
Systematic review - yet another DSM failwas invoked but never defined (see the help page). - ^ Augustine Fellowship (June 1986). Sex and Love Addicts Anonymous. Augustine Fellowship. ISBN 0-9615701-1-3. OCLC 13004050.
- ^ a b c d Cite error: The named reference
Natural and drug addictionswas invoked but never defined (see the help page). - ^ a b Cite error: The named reference
ΔFosB rewardwas invoked but never defined (see the help page). - ^ Francoeur, R. T. (1994). Taking sides: Clashing views on controversial issues in human sexuality, p. 25. Dushkin Pub. Group.
- ^ Kingston, D. A.; Firestone, P. (2008). "Problematic hypersexuality: A review of conceptualization and diagnosis". Sexual Addiction and Compulsivity. 15 (4): 284–310. doi:10.1080/10720160802289249.
- ^ Mayo Clinic Website
- ^ a b Levine, M. P.; Troiden, R. R. (1988). "The myth of sexual compulsivity". Journal of Sex Research. 25 (3): 347–363. doi:10.1080/00224498809551467.
- ^ Giles, J. (2006). "No such thing as excessive levels of sexual behavior". Archives of Sexual Behavior. 35 (6): 641–642. doi:10.1007/s10508-006-9098-3. PMID 17109229.
- ^ a b c d Klein, Marty (June–July 2003). "Sex Addiction: A Dangerous Clinical Concept" (PDF). SIECUS Report. 31 (5). ProQuest Academic Research Library: 8–11. Retrieved 15 October 2012.
- ^ Kama Sutta, Sutta Nipata 4.1
Further reading
- There are several books which offer overview history and treatment techniques for sexual addiction, including the following
- Out of the Shadows: Understanding Sex Addiction by Patrick Carnes. (Hazelden, 1983) ISBN 978-1-56838-621-8
- Sex and Love Addicts Anonymous: The Basic Text for the Augustine Fellowship (Augustine Fellowship, 1986) ISBN 978-0-9615-7011-8
- Sex Lies and Forgiveness: Couples Speaking Out on Healing from Sex Addiction by Jennifer P. Schneider and Burt Schneider. (Recovery Resources Press, 1991) ISBN 978-0-06-255343-0
- Don't Call It Love: Recovery From Sexual Addiction by Bantam, Patrick Carnes. (1992) ISBN 978-0-553-35138-5
- Sex Addiction: Case Studies And Management by Ralph H. Earle and Marcus R. Earle. (Brunner/Mazel, 1995) ISBN 978-0-87630-785-4
- Sexual Addiction: An Integrated Approach by Aviel Goodman. (International Universities Press, 1998) ISBN 978-0-8236-6063-6
- The Drug of the New Millennium: The Science of how Internet Pornography Radically Alters the Human Brain and Body by Mark B. Kastleman. (Granite Publishing and Distribution, 2001) ISBN 1930980639
- Healing the Wounds of Sexual Addiction by Mark Laaser (Zondervan, 2004) ISBN 978-0-310-25657-1
- Lust, Anger, Love: Understanding Sexual Addiction and the Road to Healthy Intimacy by Maureen Canning. (Sourcebooks, 2008) ISBN 978-1-4022-0868-3
- Erotic Intelligence: Igniting Hot, Healthy Sex While in Recovery from Sex Addiction by Alexandra Katehakis. (Health Communications, 2010) ISBN 978-0-7573-1437-7
- Cruise Control: Understanding Sex Addiction in Gay Men by Robert Weiss. (Gentle Path Press, 2011) ISBN 978-1-4596-0844-3
- Breaking the Cycle: Free Yourself from Sex Addiction, Porn Obsession, and Shame by George N. Collins, Andrew Adleman. (New Harbinger Publications, 2011) ISBN 978-1-60882-083-2
- Making Advances: A Comprehensive Guide for Treating Female Sex and Love Addictions (SASH, 2012) ISBN 978-0-9857-4720-6
- There are also books focusing on partners of sex addicts
- My Secret Life with a Sex Addict – from discovery to recovery by Emma Dawson. (Thornton Publishing, 2004) ISBN 978-1-932344-70-7
- Hope After Betrayal: Healing When Sexual Addiction Invades Your Marriage by Meg Wilson. (Kregel Publications, 2007) ISBN 978-0-8254-3935-3
- Deceived: Facing Sexual Betrayal Lies and Secrets by Claudia Black. (Hazelden, 2009) ISBN 978-1-59285-698-5
- Your Sexually Addicted Spouse: How Partners Can Cope and Heal by Barbara Steffens and Marsha Means. (New Horizon Press, 2009) ISBN 978-0-88282-309-6
- Mending a Shattered Heart: A Guide for Partners of Sex Addicts by Stefanie Carnes. (Gentle Path Press, 2011) ISBN 978-0-9774400-6-1
- Love You, Hate the Porn: Healing a Relationship Damaged by Virtual Infidelity by Mark Chamberlain. (Shadow Mountain; 2.7.2011 edition, 2011. ISBN 1606419366
- A Couple's Guide to Sexual Addiction: A Step-by-Step Plan to Rebuild Trust and Restore Intimacy by Paldrom Collins and George Collins. (Adams Media, 2011) ISBN 978-1-4405-1221-6
- Facing Heartbreak: Steps to Recovery for Partners of Sex Addicts by Stefanie Carnes. (Gentle Path Press, 2012) ISBN 978-0-98327-133-8
- The interested reader can find discussions of the concept of sexual addiction in
- Masters, William H.; Johnson, Virginia E.; Kolodny, Robert C. (1995). "Chapter 17, the section "Sexual Addictions: Fact or Fad?"". Human Sexuality (5 ed.). Harper Collins Publishers. ISBN 9780673467850.
{{cite book}}: Cite has empty unknown parameters:|chapterurl=and|authormask=(help)
External links
- Lynne Schultz. Does Sex Addiction Exist? The Bibliography of Electronic Sources
- IAAOC: Recommended reading on sexual addictions (The International Association of Addictions and Offender Counselors)
- Sex Addiction Tests