Macular degeneration: Difference between revisions
Etan J. Tal (talk | contribs) No edit summary |
→Age-related macular degeneration: don't repeat page title |
||
| Line 20: | Line 20: | ||
Although some macular dystrophies affecting younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD). |
Although some macular dystrophies affecting younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD). |
||
== Age-related |
== Age-related== |
||
Age-related macular degeneration begins with characteristic yellow deposits in the macula (central area of the retina which provides detailed central vision, called the fovea) called [[drusen]] between the [[retinal pigment epithelium]] and the underlying [[choroid]]. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol lowering agents. |
Age-related macular degeneration begins with characteristic yellow deposits in the macula (central area of the retina which provides detailed central vision, called the fovea) called [[drusen]] between the [[retinal pigment epithelium]] and the underlying [[choroid]]. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol lowering agents. |
||
Revision as of 14:24, 9 June 2009
| Macular degeneration | |
|---|---|
| Specialty | Ophthalmology |
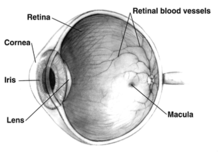


Macular degeneration is a medical condition usually of older adults which results in a loss of vision in the center of the visual field (the macula) because of damage to the retina. It occurs in “dry” and “wet” forms. It is a major cause of blindness in the elderly (>50 years)[citation needed]. Macular degeneration can make it difficult or impossible to read or recognize faces, although enough peripheral vision remains to allow other activities of daily life.
The inner layer of the eye is the retina, which contains nerves that communicate sight, and behind the retina is the choroid, which contains the blood supply to the retina. In the dry (nonexudative) form, cellular debris called drusen accumulate between the retina and the choroid, and the retina can become detached. In the wet (exudative) form, which is more severe, blood vessels grow up from the choroid behind the retina, and the retina can also become detached. It can be treated with laser coagulation, and with medication that stops and sometimes reverses the growth of blood vessels.[1][2]
Although some macular dystrophies affecting younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD).
Age-related macular degeneration begins with characteristic yellow deposits in the macula (central area of the retina which provides detailed central vision, called the fovea) called drusen between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol lowering agents.
Researchers from the University of Southampton reported October 7, 2008 that they had discovered six mutations of the gene SERPING1 that are associated with AMD. Mutations in this gene can also cause hereditary angioedema.[3]
Advanced AMD, which is responsible for profound vision loss but never total blindness, has two forms: dry and wet. Central geographic atrophy, the “dry” form of advanced AMD, results from atrophy to the retinal pigment epithelial layer below the retina, which causes vision loss through loss of photoreceptors (rods and cones) in the central part of the eye. While no treatment is available for this condition, vitamin supplements with high doses of antioxidants, lutein and zeaxanthin, have been suggested by the National Eye Institute and others to slow the progression of dry macular degeneration and, in some patients, improve visual acuity.[4]
Neovascular or exudative AMD, the “wet” form of advanced AMD, causes vision loss due to abnormal blood vessel growth in the choriocapillaries, through Bruch's membrane, ultimately leading to blood and protein leakage below the macula. Bleeding, leaking, and scarring from these blood vessels eventually cause irreversible damage to the photoreceptors and rapid vision loss if left untreated.
Until recently, no effective treatments were known for wet macular degeneration. However, new drugs, called anti-angiogenics or anti-VEGF (anti-Vascular Endothelial Growth Factor) agents, can cause regression of the abnormal blood vessels and improvement of vision when injected directly into the vitreous humor of the eye. The injections can be painful and frequently have to be repeated on a monthly or bi-monthly basis. Examples of these agents include Lucentis, Avastin (a close chemical relative of Lucentis) and Macugen. Only Lucentis and Macugen are approved by the FDA for AMD as of April 2007. Avastin is approved, but for other indications. Macugen has been found to have only minimal benefits in neovascular AMD and is no longer used. Worldwide, Avastin has been used extensively despite its "off label" status. The cost of Lucentis is approximately US$3000 per treatment while the cost of Avastin is approximately US$150 per treatment. Both drugs are made by Genentech.
Risk factors
- Aging: Approximately 10% of patients 66 to 74 years of age will have findings of macular degeneration. The prevalence increases to 30% in patients 75 to 85 years of age.[5]
- Family history: The lifetime risk of developing late-stage macular degeneration is 50% for people who have a relative with macular degeneration, versus 12% for people who do not have relatives with macular degeneration, a fourfold higher risk.[5]
- Macular degeneration gene: The genes for the complement system proteins factor H (CFH) and factor B (CFB) and factor 3 (C3) have been determined to be strongly associated with a person's risk for developing macular degeneration. CFH is involved in inhibiting the inflammatory response mediated via C3b (and the Alternative Pathway of complement) both by acting as a cofactor for cleavage of C3b to its inactive form, C3bi, and by weakening the activecomplex that forms between C3b and factor B. C-reactive protein and polyanionic surface markers such as glycosaminoglycans normally enhance the ability of factor H to inhibit complement . But the mutation in CFH(Tyr402His) reduces the affinity of CFH for CRP and probably also alters the ability of factor H to recognise specific glycosaminoglycans. This changeresults in reduced ability of CFH to regulate complement on critical surfaces such as the specialised membrane at the back of the eye and leads to increased inflammatory response within the macula. In two 2006 studies at YaleDepartment of Epidemiology and Public Health and the Department of Ophthalmology and Visual Sciences, Moran Eye Center at the University of Utah School of Medicine, another gene that has implications for the disease, called HTRA1 (encoding a secreted serine protease), was identified. [6][7]
The mitochondrial genome (mtDNA) in humans is contained on a single circular chromosome 16,569 basepairs around, and each mitochondrion contains 5 to 10 copies of the mitochondrial chromosome. There are several essential genes in mtDNA that are involved in replication and translation, along with some genes that are crucial for the machinery that converts metabolic energy into ATP. These include NADH dehydrogenase, cytochrome c oxidase, ubiquinol/cytochrome c oxidoreductase, and ATP synthase, as well as the genes for unique Ribosomal RNA and Transfer RNA particles that are required for translating these genes into proteins.
There are specific diseases associated with mutations in some of these genes. Below is one of the affected genes and the disease which arises from its mutation.- Mutation of the ATP synthase gene: Retinitis Pigmentosa (RP) is a genetically linked dysfunction of the retina and is related to mutation of the Adenosine Tri-Phosphate (ATP) Synthase Gene 615.1617
- Stargardt’s disease (STGD, also known as Juvenile Macular Degeneration) is an autosomal recessive retinal disorder characterized by a juvenile-onset macular dystrophy, alterations of the peripheral retina, and subretinal deposition of lipofuscin-like material. A gene encoding an ATP-binding cassette (ABC) transporter was mapped to the 2-cM (centiMorgan) interval at 1p13-p21 previously shown by linkage analysis to harbor the STGD gene. This gene, ABCR, is expressed exclusively and at high levels in the retina, in rod but not cone photoreceptors, as detected by in situ hybridization. Mutational analysis of ABCR in STGD families revealed a total of 19 different mutations including homozygous mutations in two families with consanguineous parentage. These data indicate that ABCR is the causal gene of STGD/FFM.
- Drusen CMSD studies indicate that drusen are similar in molecular composition to plaques and deposits in other age-related diseases such as Alzheimer's disease and atherosclerosis.
While there is a tendency for drusen to be blamed for the progressive loss of vision, drusen deposits can, however, be present in the retina without vision loss. Some patients with large deposits of drusen have normal visual acuity. If normal retinal reception and image transmission are sometimes possible in a retina when high concentrations of drusen are present, then even if drusen can be implicated in the loss of visual function, there must be at least one other factor that accounts for the loss of vision. Retinitis Pigmentosa (RP) is a genetically linked dysfunction of the retina and is related to mutation of the ATP Synthase Gene 63.
- Arg80Gly variant of the complement protein C3 Two independent genetic studies from two groups published in the New England Journal of Medicine and Nature Genetics in 2007 showed that a certain, common mutation in the C3 gene which is a central protein of the complement system is strongly associated with the occurrence of Age-related Macular Degeneration.[8][9] The authors of both papers consider their study to underscore the influence of the complement pathway in the pathogenesis of this disease.
- Hypertension: Also known as high blood pressure.
- Cardiovascular status — high cholesterol, obesity.
- High fat intake is associated with an increased risk of macular degeneration in both women and men. Fat provides about 42% of the food energy in the average American diet. A diet that derives closer to 20-25% of total food energy from fat is probably healthier. Reducing fat intake to this level means cutting down greatly on consumption of red meats and high-fat dairy products such as whole milk, cheese, and butter. Eating more cold-water fish[10] (at least twice weekly), rather than red meats, and eating any type of nuts may help macular degeneration patients.[11]
- Oxidative stress: It has been proposed that age related accumulation of low molecular weight, phototoxic, pro-oxidant melanin oligomers within lysosomes in the retinal pigment epithelium may be partly responsible for decreasing the digestive rate of photoreceptor outer rod segments (POS) by the RPE. A decrease in the digestive rate of POS has been shown to be associated with lipofuscin formation - a classic sign associated with macular degeneration.[12][13]
- Fibulin-5 mutation Rare forms of the disease are caused by geneic defects in fibulin-5, in an autosomal dominant manner. In 2004 Stone et al. performed a screen on 402 AMD patients and revealed a statistically significant correlation between mutations in Fibulin-5 and incidence of the disease. Furthermore the point mutants were found in the Calcium binding sites of the cbEGF domains of the protein. there is no structural basis for the effects of the mutations.
- Race Macular degeneration is more likely to be found in Caucasians than in people of African descent.[14][15]
- Exposure to sunlight especially blue light. There is conflicting evidence as to whether exposure to sunlight contributes to the development of macular degeneration. A recent study in the British Journal of Ophthalmology on 446 subjects found that it does not.[16] Other research, however, has shown that High-energy visible light (HEV) may contribute to age-related macular degeneration.[17][18][19]
- Smoking Smoking tobacco increases the risk of macular degeneration by two to three times that of someone who has never smoked, and may be the most important modifiable factor in its prevention. A review of previous studies found that "the literature review confirmed a strong association between current smoking and AMD. ... Cigarette smoking is likely to have toxic effects on the retina." [20]
Signs
- Drusen
- Pigmentary alterations
- Exudative changes: hemorrhages in the eye, hard exudates, subretinal/sub-RPE/intraretinal fluid
- Atrophy: incipient and geographic
- Visual acuity drastically decreasing (two levels or more) ex: 20/20 to 20/80.
Symptoms
- Blurred vision: Those with nonexudative macular degeneration may be asymptomatic or notice a gradual loss of central vision, whereas those with exudative macular degeneration often notice a rapid onset of vision loss.
- Central scotomas (shadows or missing areas of vision)
- Distorted vision (i.e. metamorphopsia) - A grid of straight lines appears wavy and parts of the grid may appear blank. Patients often first notice this when looking at mini-blinds in their home.
- Trouble discerning colors; specifically dark ones from dark ones and light ones from light ones.
- Slow recovery of visual function after exposure to bright light
- A loss in contrast sensitivity.
The Amsler Grid Test is one of the simplest and most effective methods for patients to monitor the health of the macula. The Amsler Grid is essentially a pattern of intersecting lines (identical to graph paper) with a black dot in the middle. The central black dot is used for fixation (a place for the eye to stare at). With normal vision, all lines surrounding the black dot will look straight and evenly spaced with no missing or odd looking areas when fixating on the grid's central black dot. When there is disease affecting the macula, as in macular degeneration, the lines can look bent, distorted and/or missing. See a video on how to use an Amsler grid here: [1] and watch an animation showing the Amsler grid with macular degeneration here: [2].
Macular degeneration by itself will not lead to total blindness. For that matter, only a very small number of people with visual impairment are totally blind. In almost all cases, some vision remains. Other complicating conditions may possibly lead to such an acute condition (severe stroke or trauma, untreated glaucoma, etc.), but few macular degeneration patients experience total visual loss.[21] The area of the macula comprises about 5% of the retina and is responsible for about 35% of the visual field. The remaining 65% (the peripheral field) remains unaffected by the disease.[22]
The loss of central vision profoundly affects visual functioning. It is not possible, for example, to read without central vision. Pictures which attempt to depict the central visual loss of macular degeneration with a black spot do not really do justice to the devastating nature of the visual loss. This can be demonstrated by printing letters 6 inches high on a piece of paper and attempting to identify them while looking straight ahead and holding the paper slightly to the side. Most people find this surprisingly difficult to do.
There is a loss off contrast sensitivity, so that contours, shadows and color vision are less vivid. The loss in contrast sensitivity can be quickly and easily measured by a contrast sensitivity test performed either at home or by an eye specialist.
Similar symptoms with a very different etiology and different treatment can be caused by Epiretinal membrane or macular pucker or leaking blood vessels in the eye..
Diagnosis
Fluorescein angiography allows for the identification and localization of abnormal vascular processes. Optical coherence tomography is now used by most ophthalmologists in the diagnosis and the followup evaluation of the response to treatment by using either Avastin or Lucentis which are injected into the vitreous of the eye at various intervals.
Prevention
The Age-Related Eye Disease Study showed that a combination of high-dose beta-carotene, vitamin C, vitamin E, and zinc can reduce the risk of progressing from early to advanced AMD by about 25 percent.[23] Studies are underway with the goal of reducing lipofuscin accumulation. [13]
Studies have found that Lutein and zeaxanthin (Carotenoid nutrients found in green vegetables such as Kale, Spinach, Collards, spices such as Saffron and egg yolk) protect against and possibly reverse macular degeneration and Retinitis pigmentosa.[24][25] Studies found that antioxidants disrupt the link of two processes that cause macular degeneration and extend the lifetime of irreplaceable photoreceptors and other retinal cells (Lutein is known to have antioxidant properties). [26][27]
Eating spinach or collard greens five times a week decreases the risk of AMD by 43% (27)
Impact
Macular degeneration can advance to legal blindness and inability to drive. It can also result in difficulty or inability to read or see faces.
Adaptive devices can help people read. These include magnifying glasses, special eyeglass lenses, desktop and portable electronic devices, and computer screen readers such as JAWS for Windows.

Accessible publishing also aims to provide a variety of fonts and formats for published books to make reading easier. This includes much larger fonts for printed books, patterns to make tracking easier, audiobooks and DAISY books with both text and audio.
Because the peripheral vision is not affected, people with macular degeneration can learn to use their remaining vision to continue most activities. Assistance and resources are available in every country and every state in the U.S. Classes for "independent living" are given and some technology can be obtained from a state department of rehabilitation. You can also search for macular degeneration on the internet and contact one of the non-profit organizations for assistance.
References
- ^ de Jong PT (2006). "Age-related macular degeneration". N Engl J Med. 355 (14): 1474–1485. doi:10.1056/NEJMra062326. PMID 17021323.
- ^ Ch. 25, Disorders of the Eye, Jonathan C. Horton, in Harrison's Principles of Internal Medicine, 16th ed.
- ^ Hirschler, Ben (2008-10-07). "Gene discovery may help hunt for blindness cure". Reuters. Retrieved 2008-10-07.
- ^ Tan JS, Wang JJ, Flood V, Rochtchina E, Smith W, Mitchell P. (Feb 2008). "Dietary antioxidants and the long-term incidence of age-related macular degeneration: the Blue Mountain Eye Study". Ophthalmology. 115 (no. 2): 334–41. PMID 17664009.
{{cite journal}}:|issue=has extra text (help); Cite has empty unknown parameter:|1=(help)CS1 maint: multiple names: authors list (link) - ^ a b http://www.agingeye.net/maculardegen/maculardegeninformation.php
- ^ Yang Z, Camp NJ, Sun H, Tong Z, Gibbs D, Cameron DJ, Chen H, Zhao Y, Pearson E, Li X, Chien J, Dewan A, Harmon J, Bernstein PS, Shridhar V, Zabriskie NA, Hoh J, Howes K, Zhang K. "A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration." Science. 2006 Nov 10;314(5801):992-3. PMID 17053109.
- ^ Dewan A, Liu M, Hartman S, Zhang SS, Liu DT, Zhao C, Tam PO, Chan WM, Lam DS, Snyder M, Barnstable C, Pang CP, Hoh J. "A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration". Science. 2006 Nov 10;314(5801):989-92. PMID 17053108
- ^ Yates JR, Sepp T, Matharu BK, Khan JC, Thurlby DA, Shahid H, Clayton DG, Hayward C, Morgan J, Wright AF, Armbrecht AM, Dhillon B, Deary IJ, Redmond E, Bird AC, Moore AT (2007). "Complement C3 Variant and the Risk of Age-Related Macular Degeneration". N Engl J Med. 357 (6): 553–561. doi:10.1056/NEJMoa072618. PMID 17634448.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Maller JB, Fagerness JA, Reynolds RC, Neale BM, Daly MJ, Seddon JM (2007). "Variation in Complement Factor 3 is Associated with Risk of Age-Related Macular Degeneration". Nature Genetics. 39 (10): 1200–1201. doi:10.1038/ng2131.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ John Paul SanGiovanni, ScD; Emily Y. Chew, MD; Traci E. Clemons, PhD; Matthew D. Davis, MD; Frederick L. Ferris III, MD; Gary R. Gensler, MS; Natalie Kurinij, PhD; Anne S. Lindblad, PhD; Roy C. Milton, PhD; Johanna M. Seddon, MD; and Robert D. Sperduto, MD (May 5, 2007). "The Relationship of Dietary Lipid Intake and Age-Related Macular Degeneration in a Case-Control Study". Archives of Ophthamology.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Macular degeneration Types and Risk Factors
- ^ "Melanin aggregation and polymerization: possible implications in age related macular degeneration." Ophthalmic Research, 2005; volume 37: pages 136-141.
- ^ a b John Lacey, "Harvard Medical signs agreement with Merck to develop potential therapy for macular degeneration", 23-May-2006
- ^ Age-Related Eye Disease Study Research Group. "Risk factors associated with age-related macular degeneration. A case-control study in the age-related eye disease study: Age-Related Eye Disease Study Report Number 3." Ophthalmology. 2000 Dec;107(12):2224-32. PMID 11097601.
- ^ Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL 3rd; Age-Related Eye Disease Study Research Group. "Risk factors for the incidence of Advanced Age-Related Macular Degeneration in the Age-Related Eye Disease Study (AREDS) AREDS report no. 19." Ophthalmology. 2005 Apr;112(4):533-9. PMID 15808240.
- ^ Khan, JC (2006). "Age related macular degeneration and sun exposure, iris colour, and skin sensitivity to sunlight". The British Journal of Ophthalmology. 90 (1): 29–32. doi:10.1136/bjo.2005.073825. PMID 16361662.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Glazer-Hockstein, C (2006). "Could blue light-blocking lenses decrease the risk of age-related macular degeneration?". Retina. 26 (1): 1–4. doi:10.1097/00006982-200601000-00001. PMID 16395131.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Margrain, TH (2004). "Do blue light filters confer protection against age-related macular degeneration?". Progress in Retinal and Eye Research. 23 (5): 523–31. doi:10.1016/j.preteyeres.2004.05.001. PMID 15302349.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Roberts, D (2005). "Artificial Lighting and the Blue Light Hazard". Macular Degeneration Support Online Library. http://www.mdsupport.org/library/hazard.html#blue.
{{cite journal}}: External link in|volume=|month=ignored (help) - ^ Smoking and age-related macular degeneration: a review of association
- ^ Roberts, DL (2006). "The First Year--Age Related Macular Degeneration". (Marlowe & Company): 100.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Roberts, DL (2006). "The First Year--Age Related Macular Degeneration". (Marlowe & Company): 20.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hoglund, T. (March 18, 2007). "Clinical Trial Finds Antioxidants and Zinc Beneficial
in Reducing Risk of Severe AMD". MD Support Online Library.
{{cite journal}}: line feed character in|title=at position 54 (help) - ^ Lutein And Zeaxanthin May Offer Protection Against MD MD Support Online Library July, 2008.
- ^ http://vision.edu.au/news/acevs%20saffron.pdf
- ^ Vives-Bauza C, Anand M, Shirazi AK, Magrane J, Gao J, Vollmer-Snarr HR, Manfredi G, Finnemann SC (July 10 2008). "The age-lipid A2E and mitochondrial dysfunction synergistically impair phagocytosis by retinal pigment epithelial cells". J Biol Chem. PMID 18621729.
{{cite journal}}: Check date values in:|date=(help); Cite has empty unknown parameter:|unused_data=(help); Text "PubMed - s supplied by publisher" ignored (help)CS1 maint: multiple names: authors list (link) - ^ Study Reveals How Diet, Antioxidants Prevent Blindness in Aging Population Newswise, Retrieved on August 19, 2008.
27 Seddon JM, Ajani UA, Sperduto RD et al. Dietary Carotenoids, Vitamin A, C and E, and Advbanced Age-Related Macular Degeneration. JAMA, 1994;272:1413-1420.
